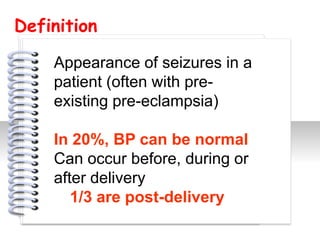
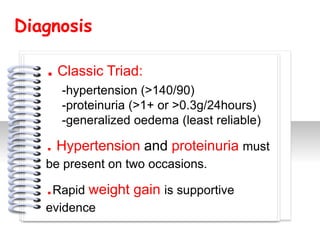
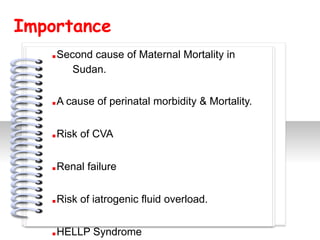
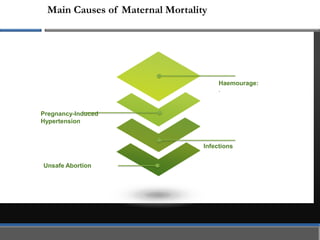
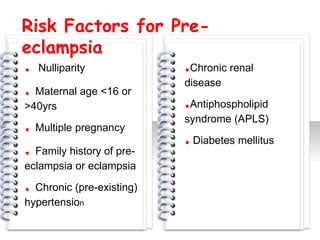
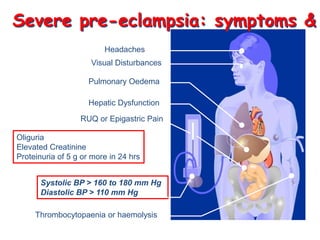
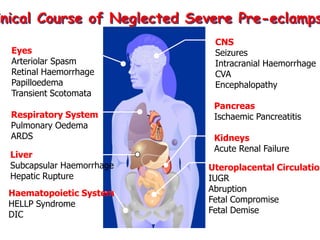
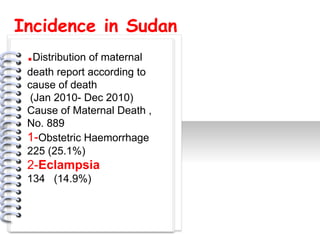
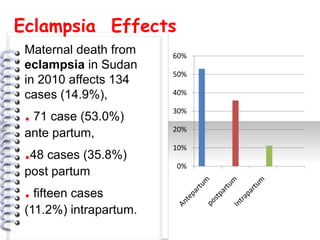
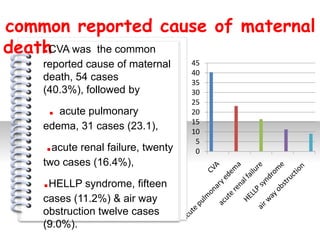
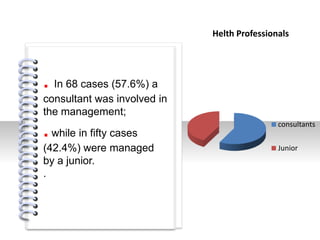
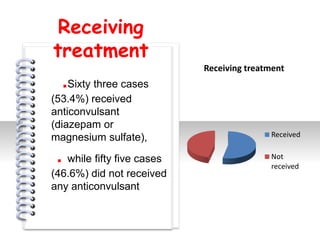
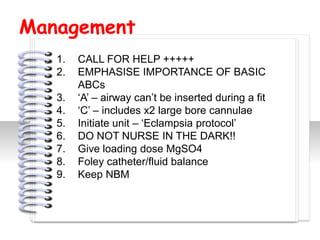
This document discusses eclampsia in Sudan. It defines eclampsia as seizures occurring in patients with pre-existing pre-eclampsia. The presentation provides details on diagnosing pre-eclampsia, risk factors, incidence in Sudan, management of severe cases, and prevention. Eclampsia is a major cause of maternal mortality in Sudan, responsible for 14.9% of deaths in 2010. Management involves anticonvulsants like magnesium sulfate, antihypertensives, and preventing future cases through availability of treatments and provider training.