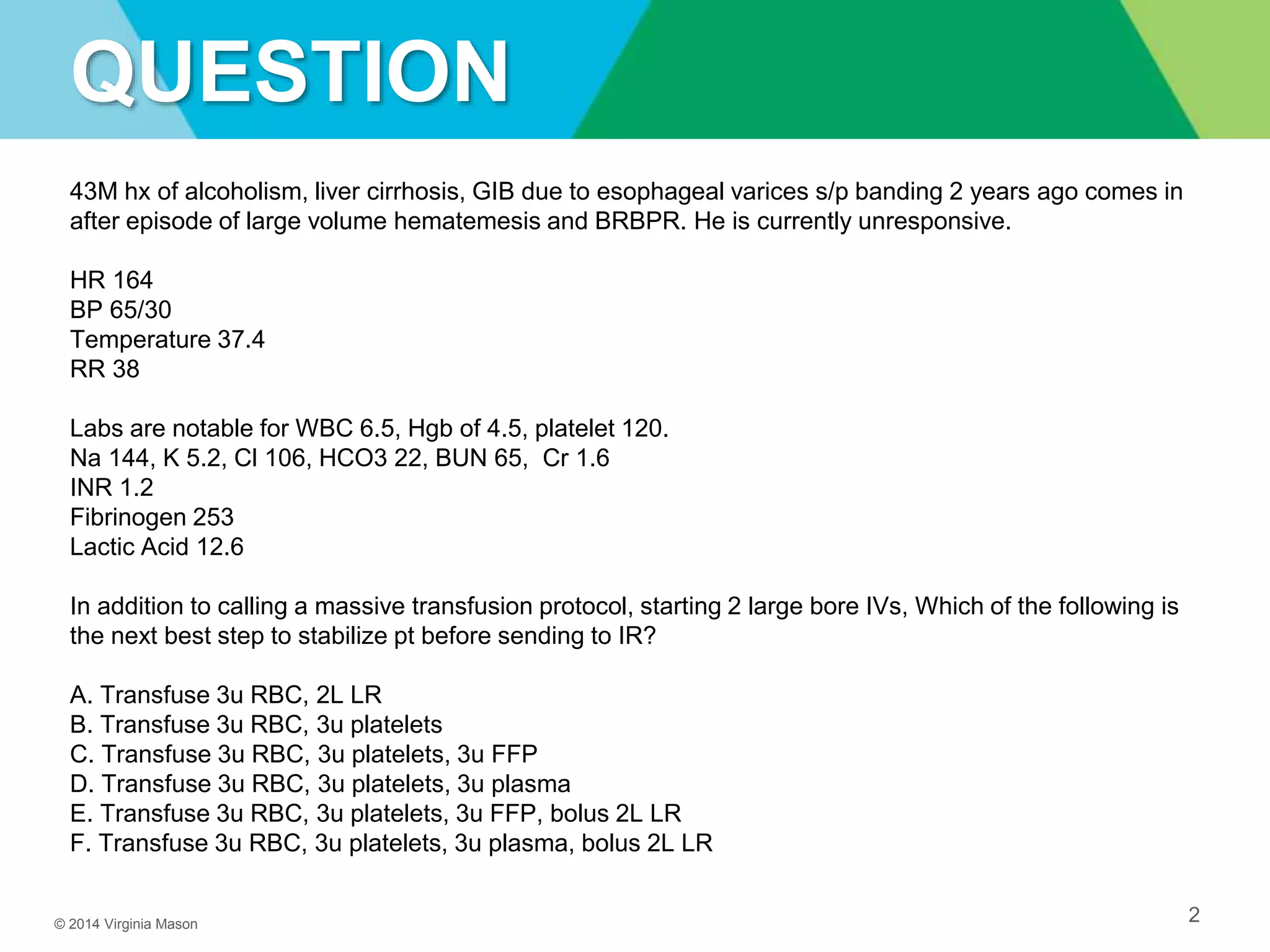
A 43-year-old man with a history of alcoholism and liver cirrhosis presented with a large gastrointestinal bleed from esophageal varices. He was unresponsive with a heart rate of 164 and low blood pressure. His labs showed anemia, thrombocytopenia, and elevated lactic acid. The next best step to stabilize the patient before transferring to interventional radiology would be to transfuse 3 units of red blood cells, 3 units of platelets, and 3 units of fresh frozen plasma while also bolusing 2 liters of lactated ringers.