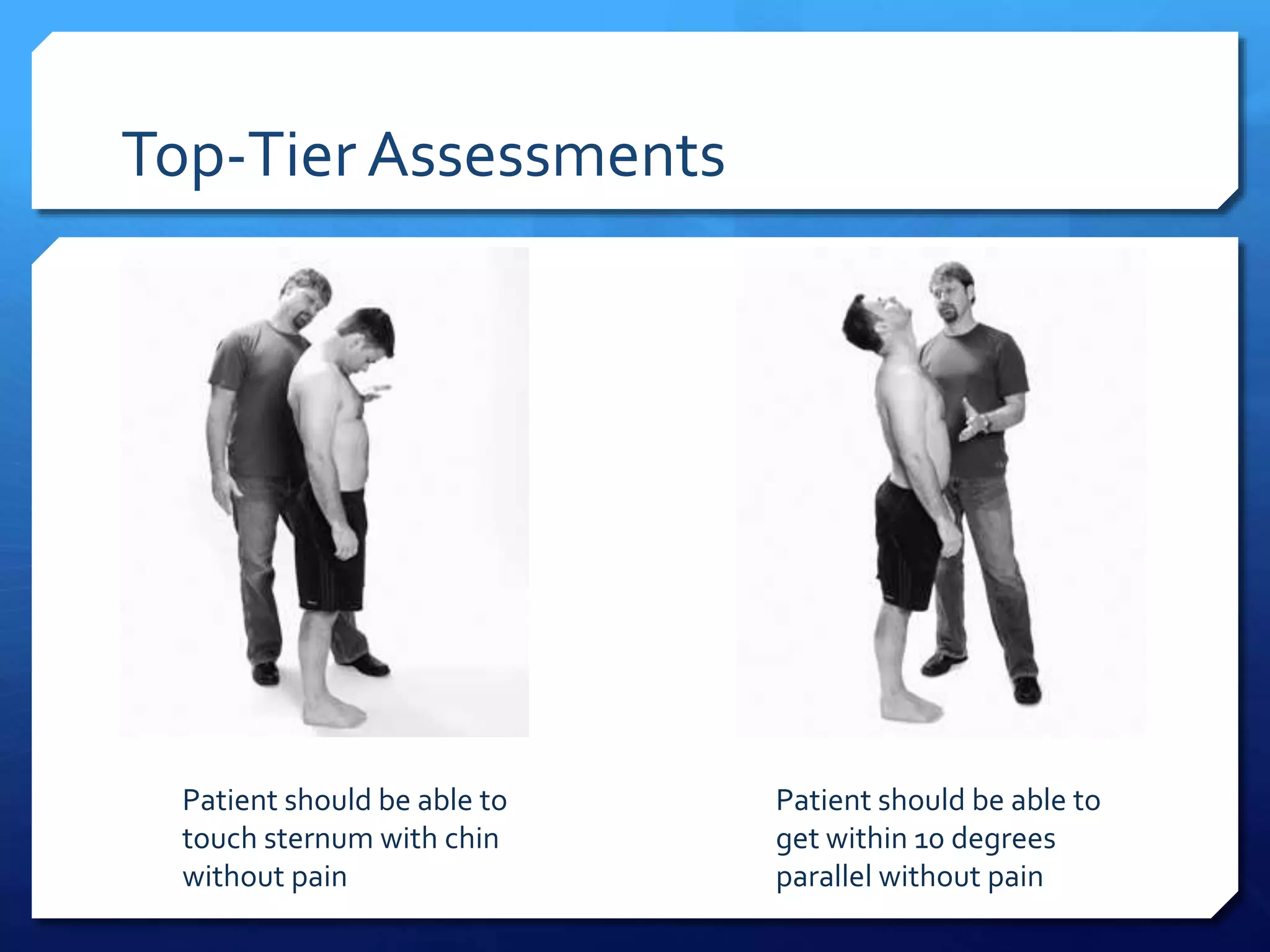
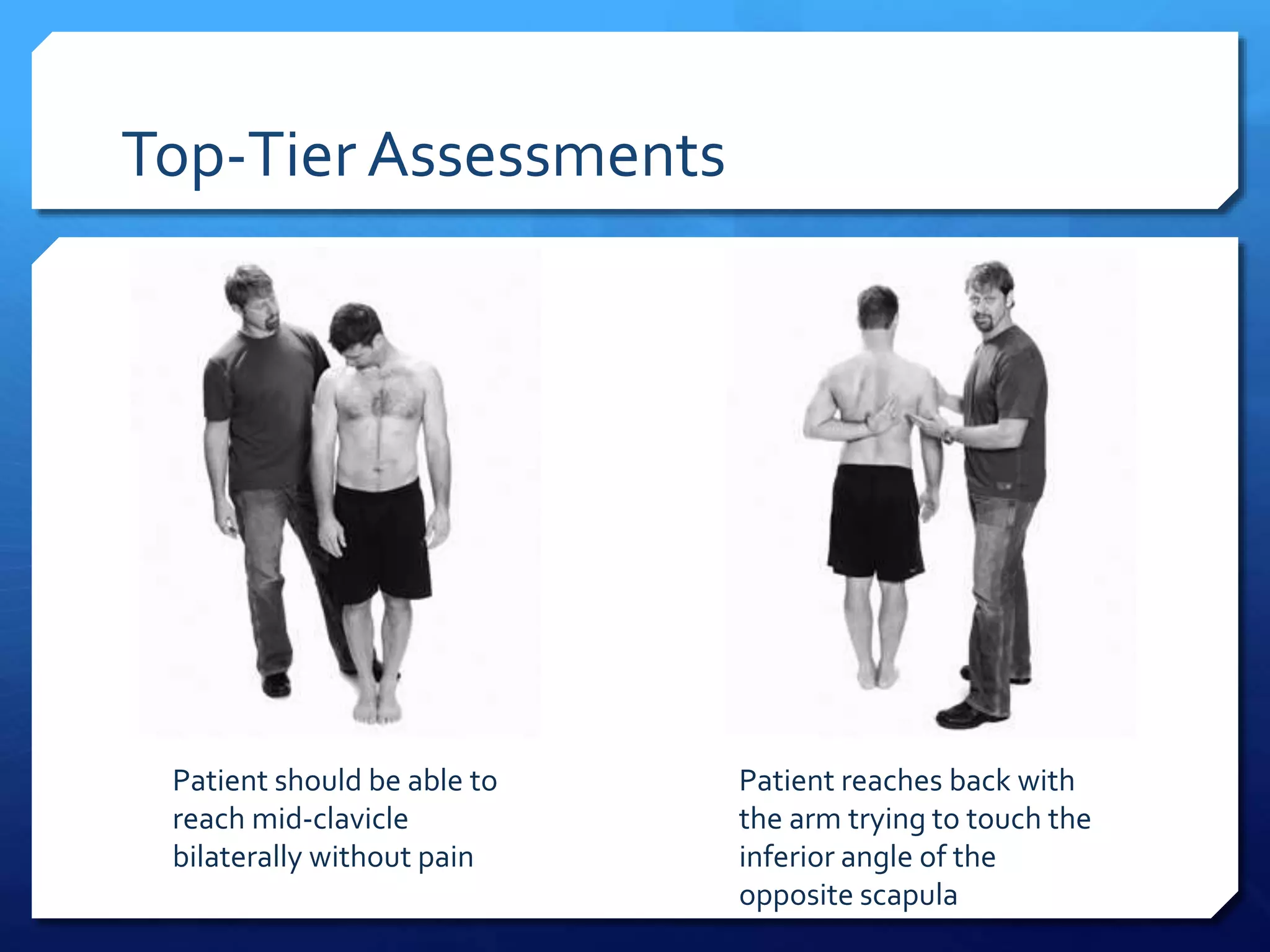
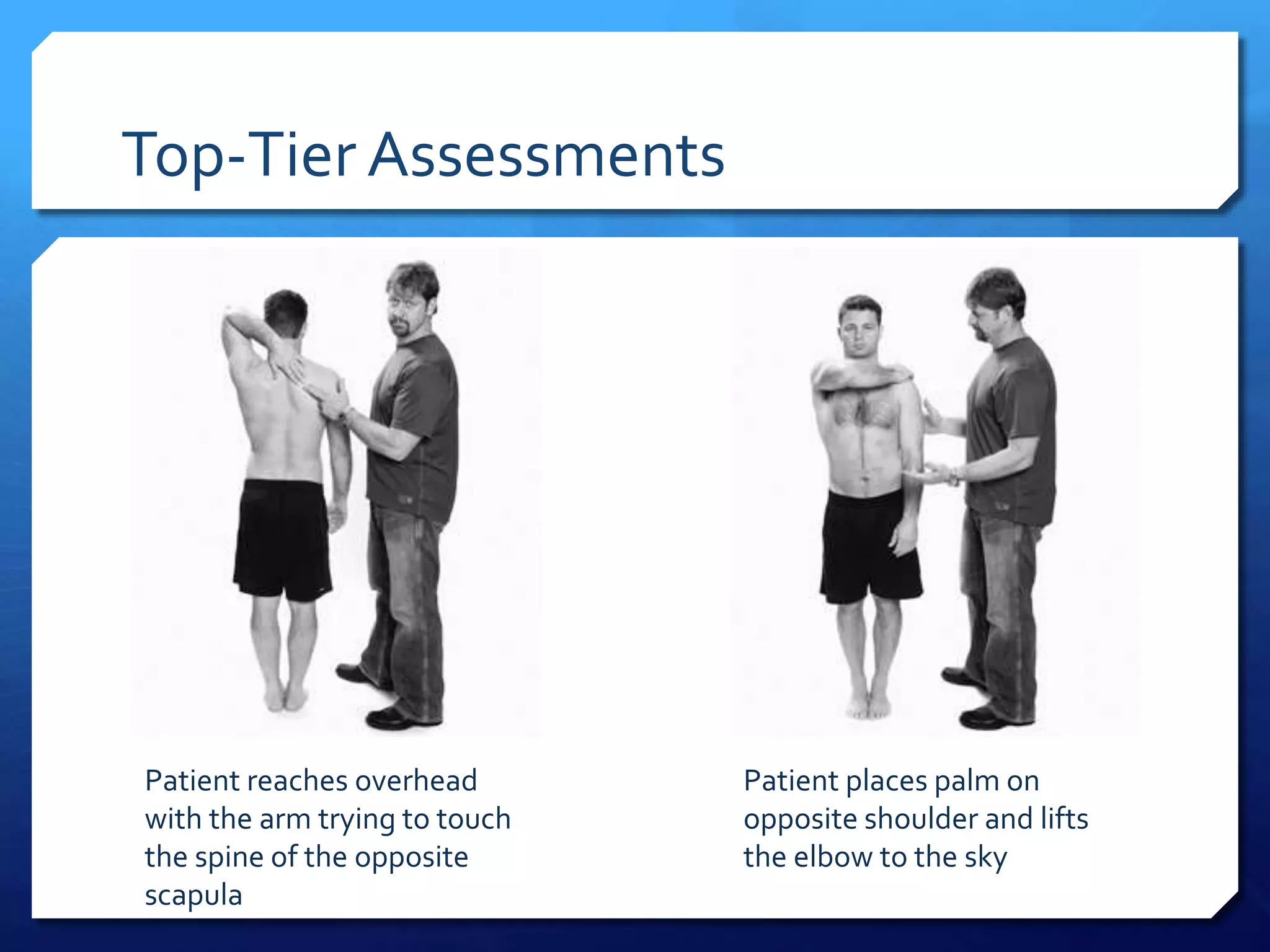
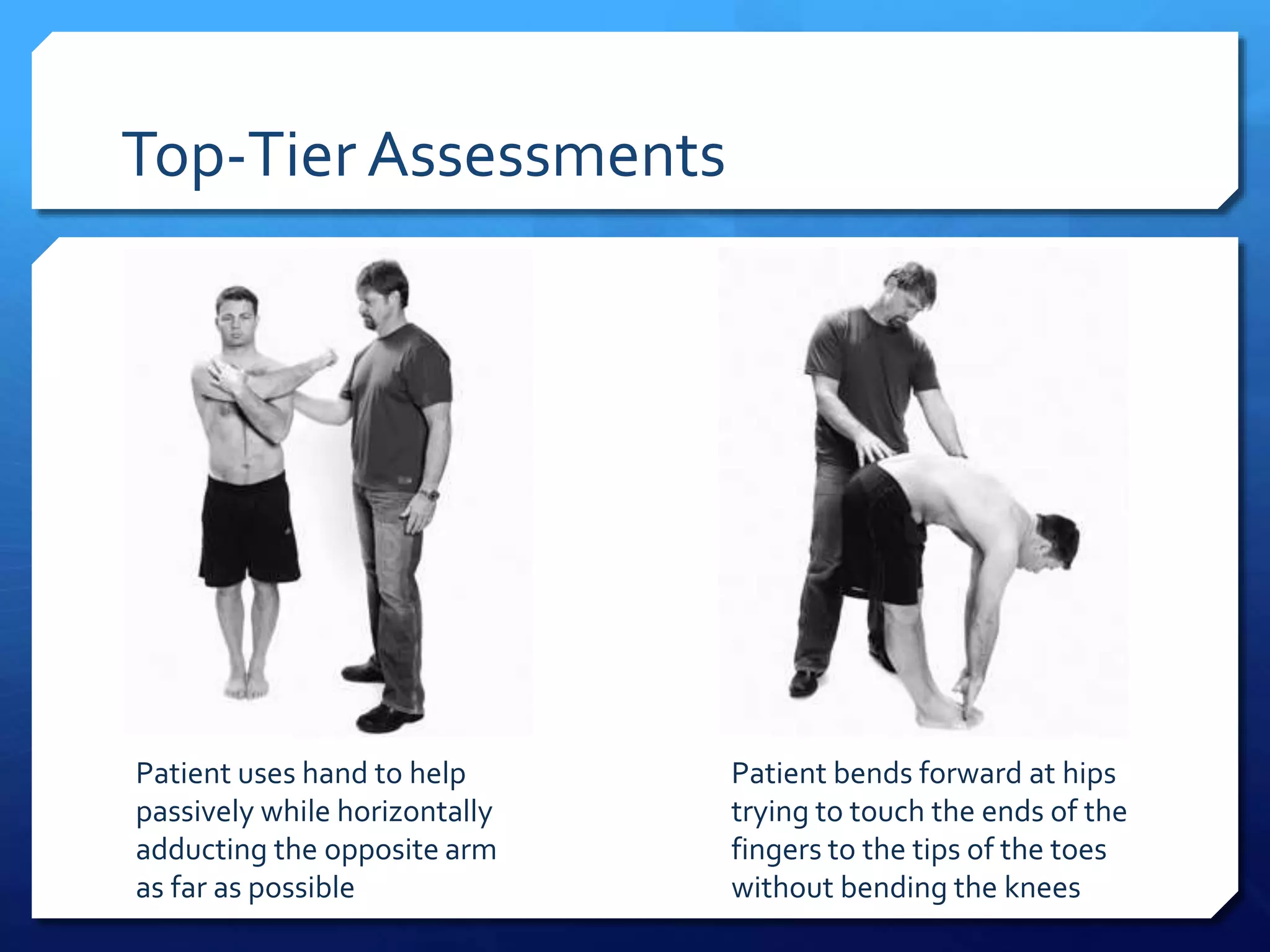
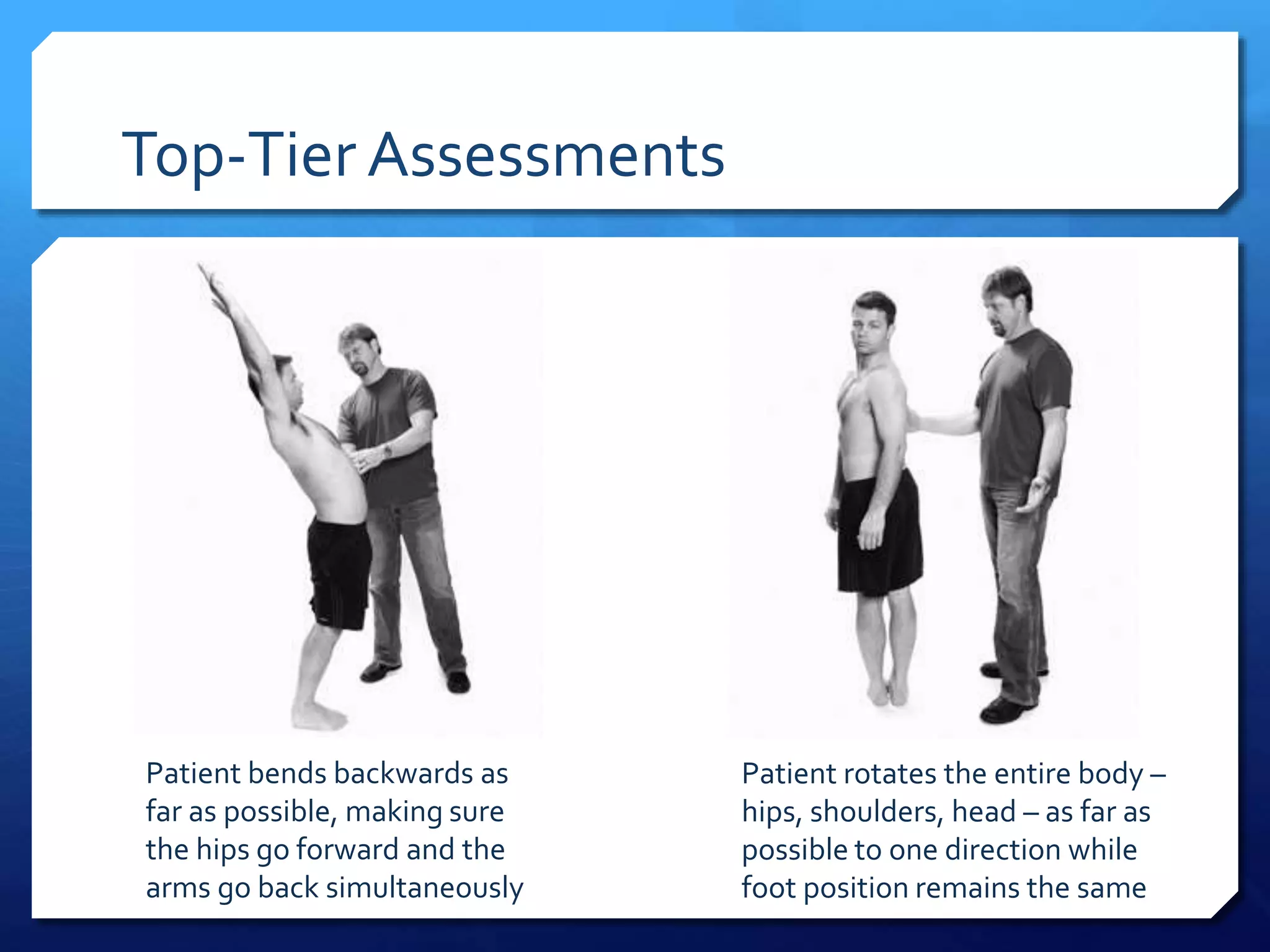
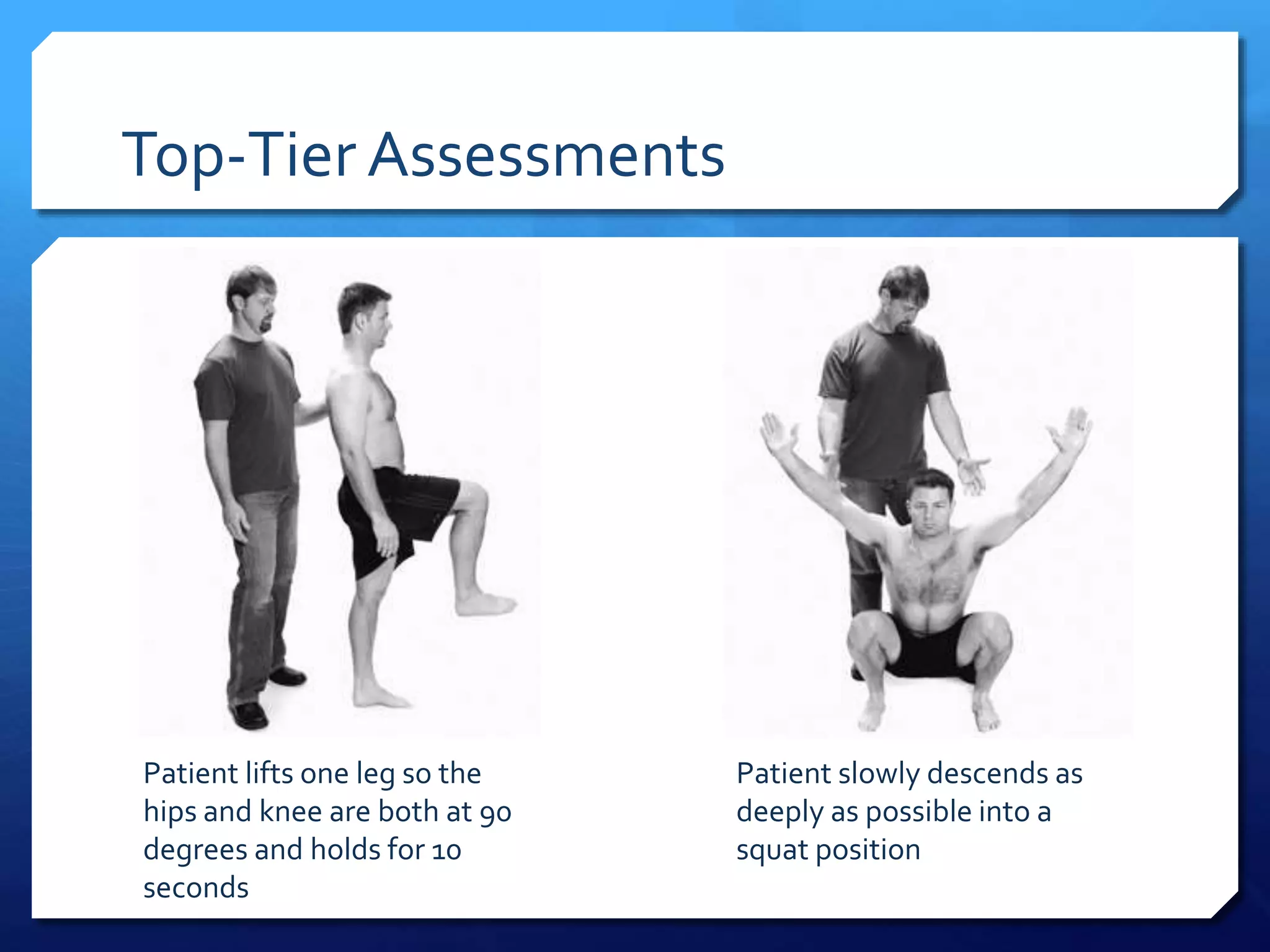
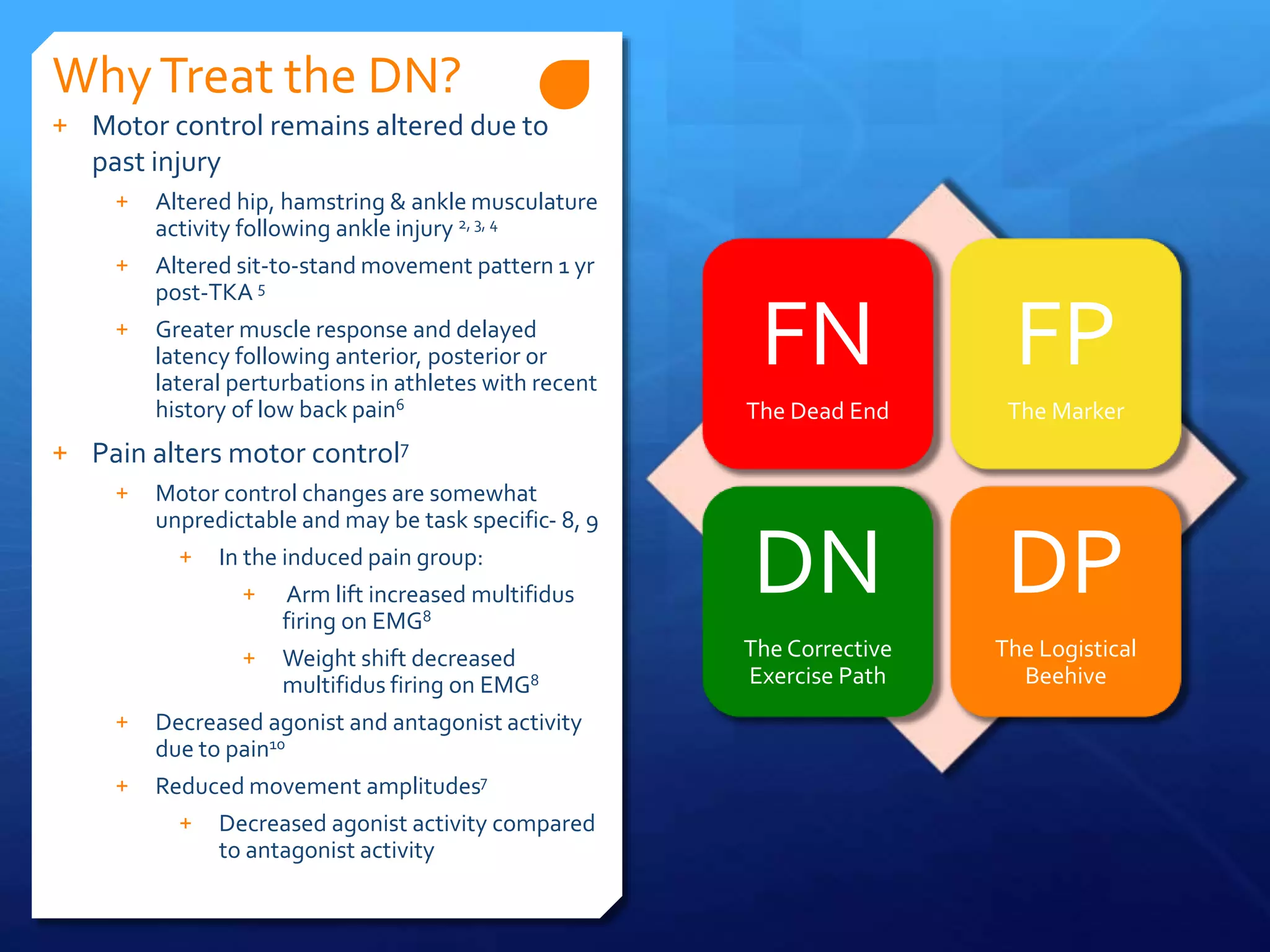
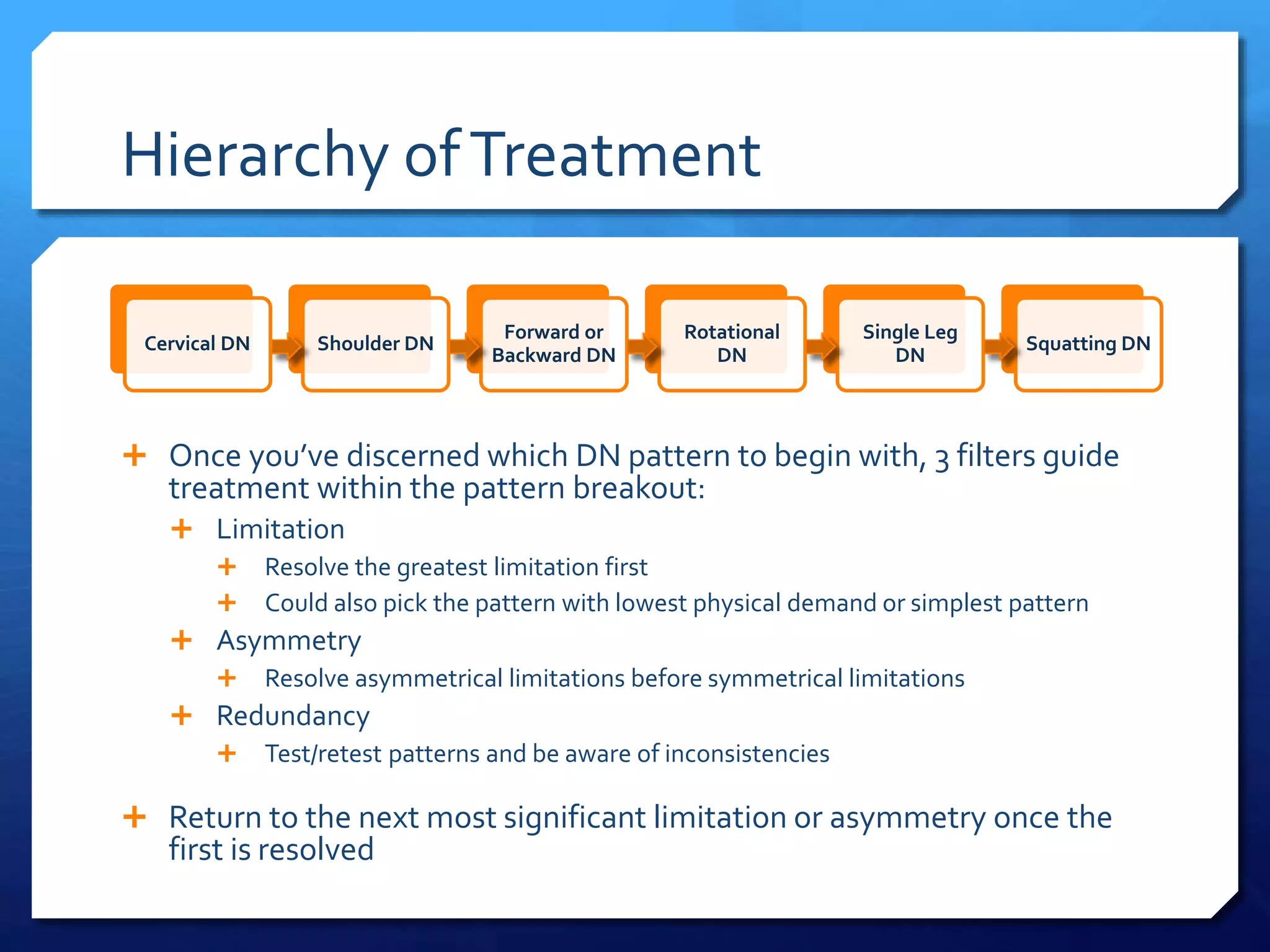
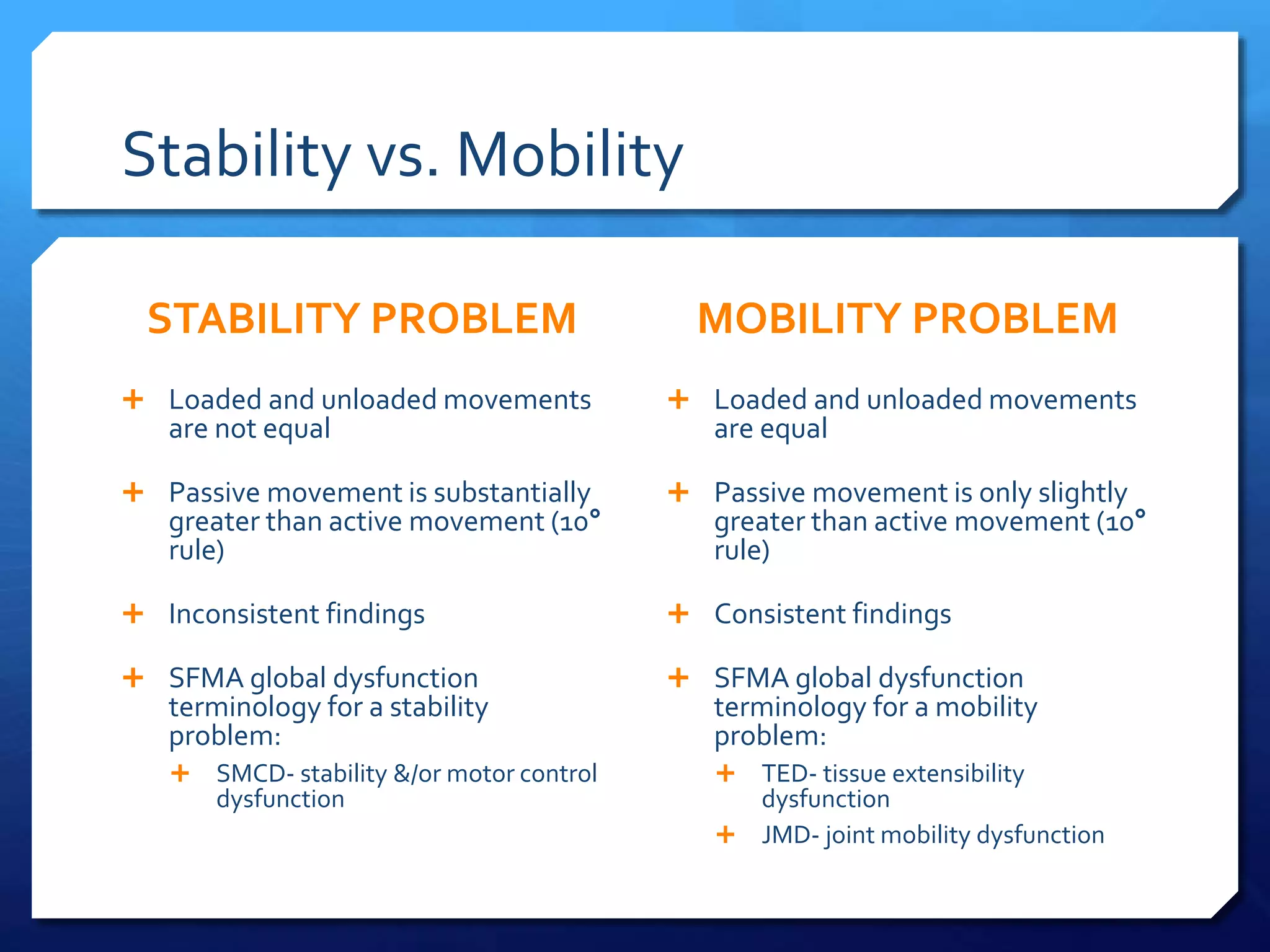
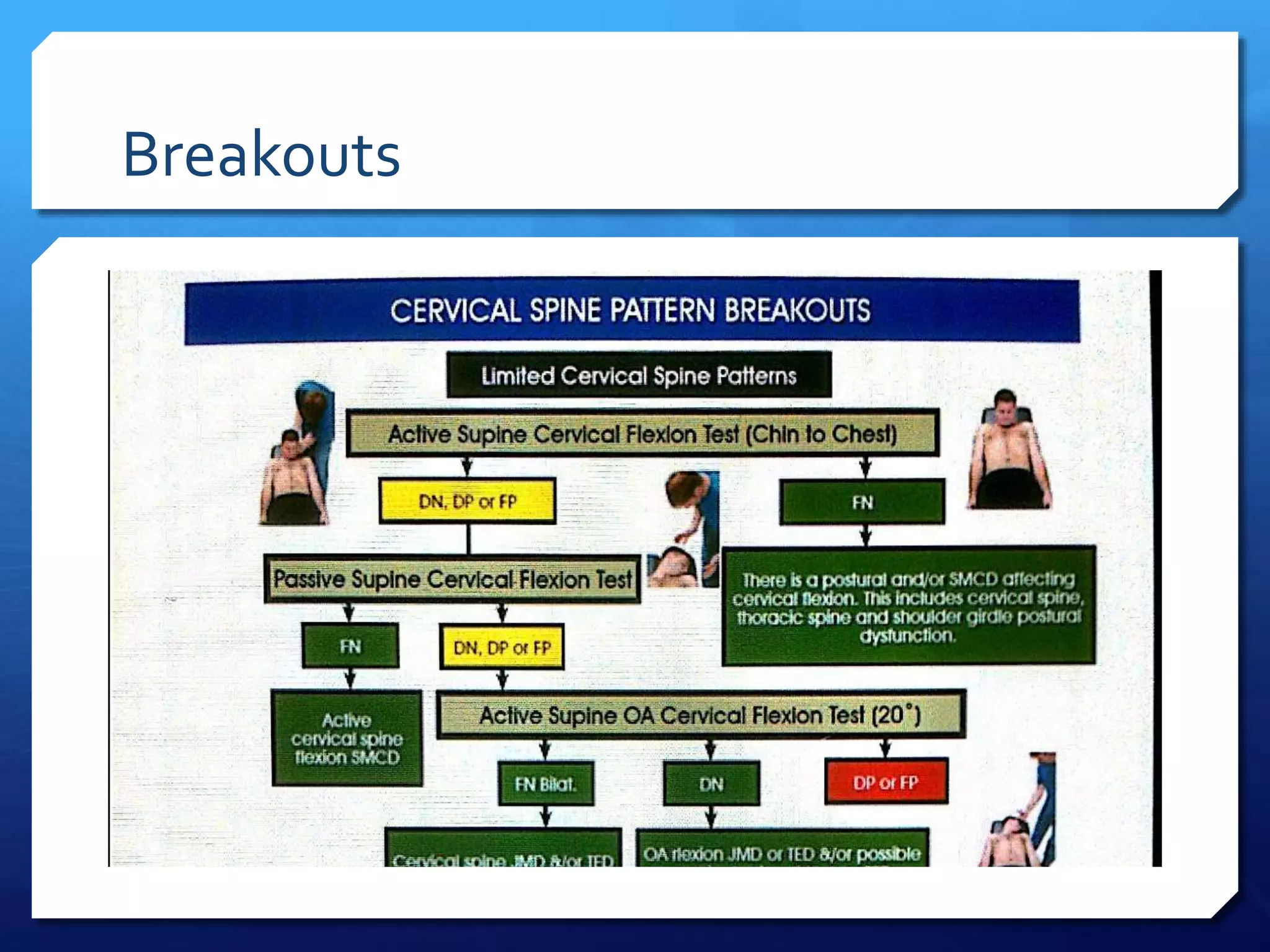
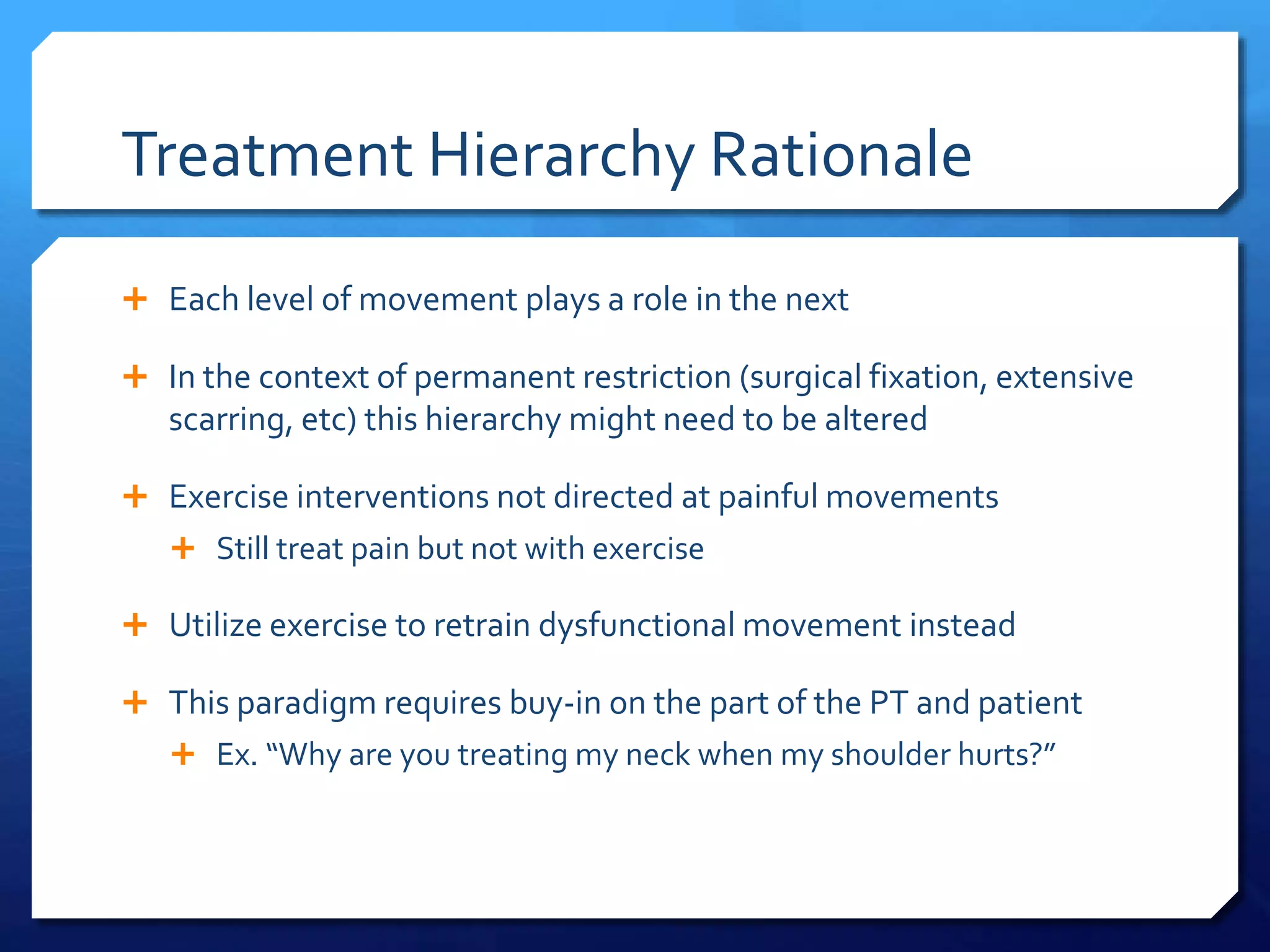
The document introduces the Selective Functional Movement Assessment (SFMA) which evaluates movement patterns and asymmetries to identify dysfunctional movement. The SFMA grades movements as functional-nonpainful, functional-painful, dysfunctional-nonpainful, or dysfunctional-painful to guide treatment. Top-tier assessments are demonstrated involving various ranges of motion. Treatment focuses on dysfunctional-nonpainful patterns using corrective exercises to improve motor control and symmetry before mobility or flexibility limitations.