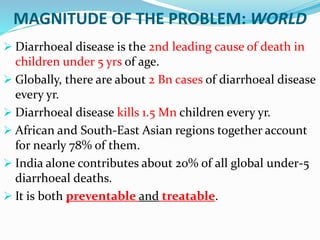
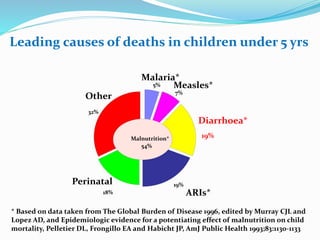
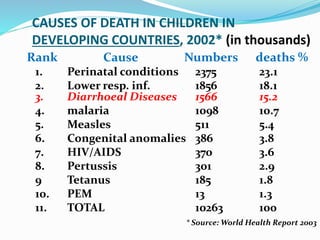
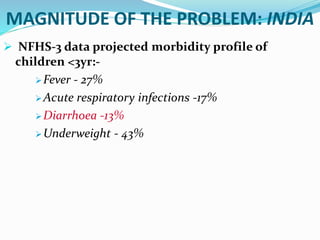
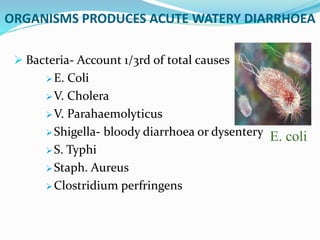
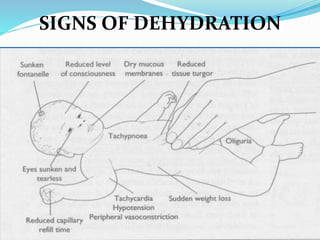
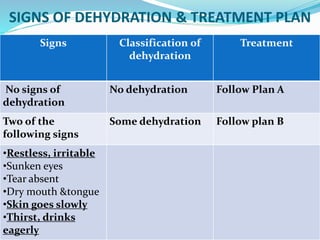
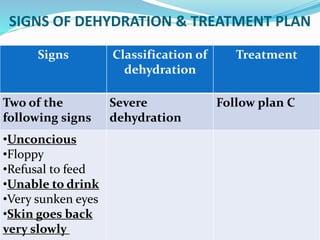
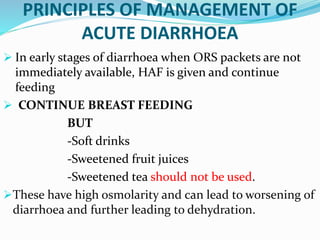
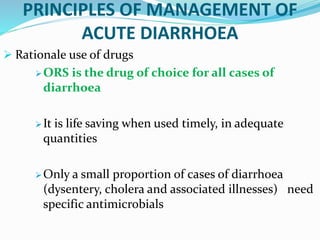
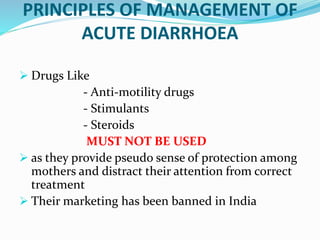
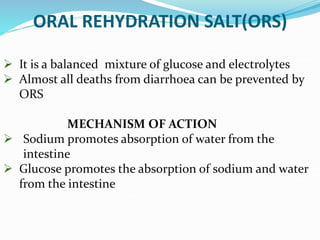
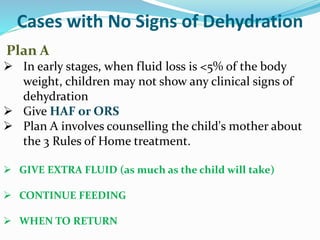
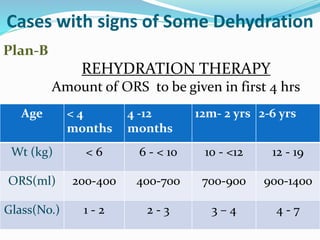
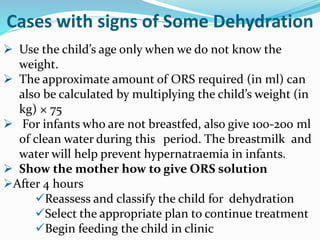
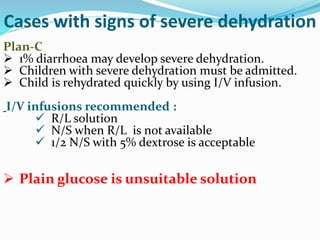
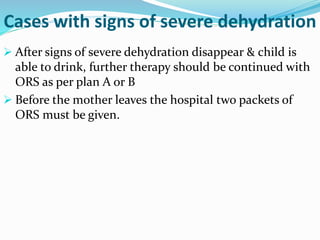
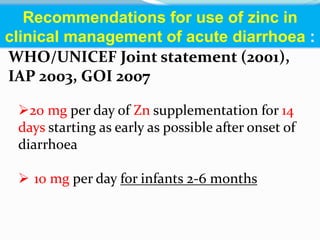
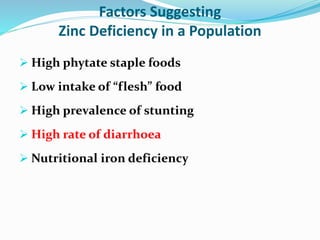
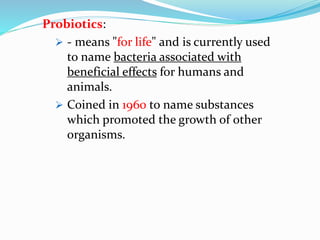
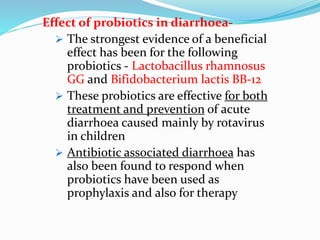
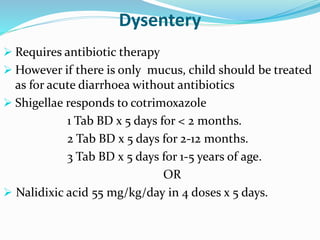
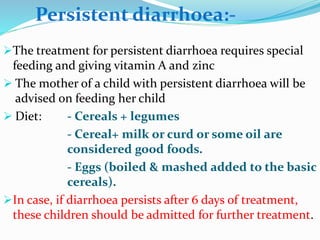
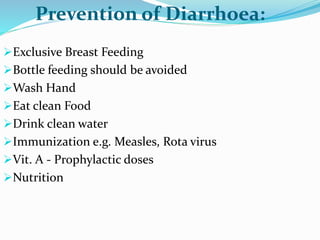
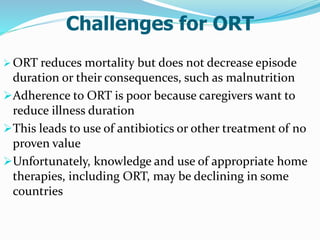
This document provides an overview of diarrheal disease including its causes, classification, management, and prevention. It discusses that diarrheal disease is the second leading cause of death in children under 5 globally. The main points are: acute watery diarrhea accounts for over 75% of cases; continued feeding and oral rehydration solutions are the primary treatment; zinc and probiotics can help prevent and treat diarrhea; and diarrhea management should focus on preventing dehydration through oral rehydration.