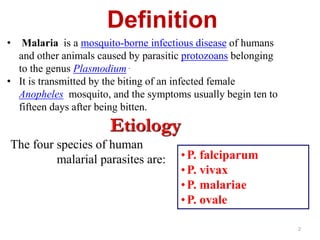
Plasmodium parasites are transmitted through the bites of infected female Anopheles mosquitoes. There are four species that cause malaria in humans. The parasite undergoes development stages in both the human and mosquito hosts. In humans, parasites first develop in the liver before infecting and destroying red blood cells. Symptoms usually appear 10-15 days after the infectious bite and include fever, chills, and flu-like illness. Laboratory diagnosis of malaria is confirmed by microscopic examination of blood films to identify the parasite. While a vaccine is still in development, current prevention strategies include antimalarial drugs for treatment, prophylaxis and rapid diagnostic tests.