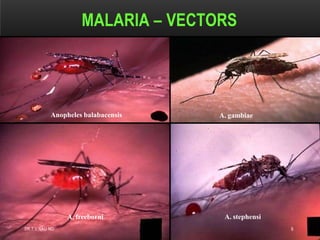
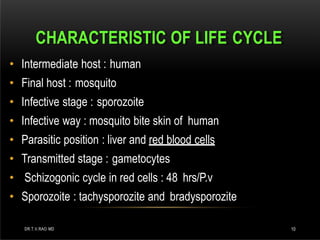
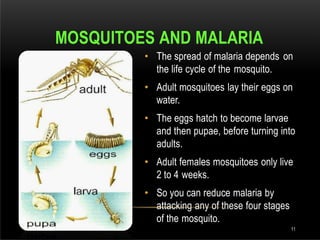
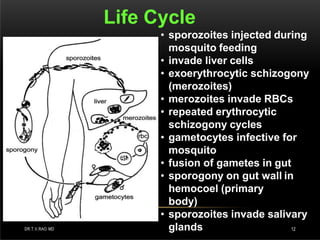
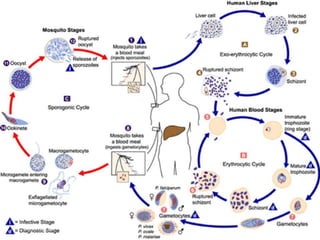
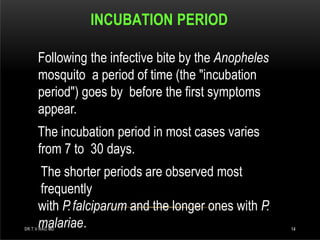
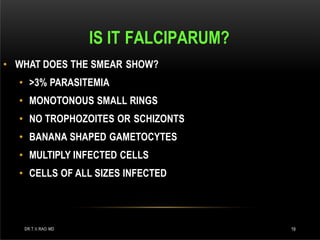
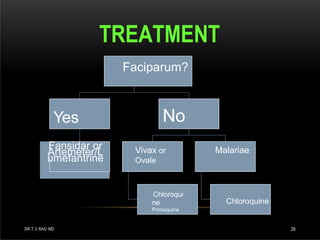
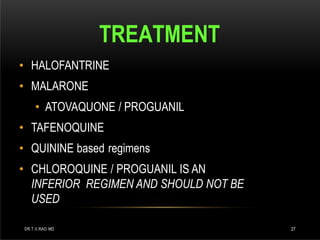
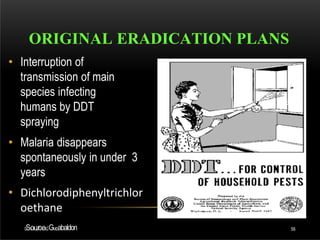
Malaria is one of the oldest infectious diseases, caused by the protozoan parasite Plasmodium and primarily transmitted by Anopheles mosquitoes. It affects 40% of the world’s population, leading to 1-2 million deaths annually, with the majority occurring in Africa. Although effective treatments like quinine exist, there is no vaccine currently available, and prevention strategies include mosquito control and medication for high-risk groups.