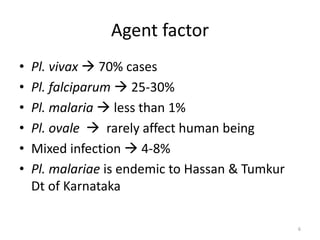
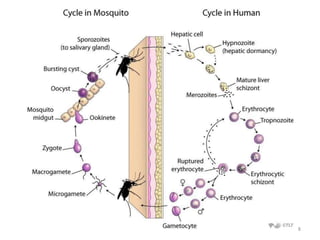
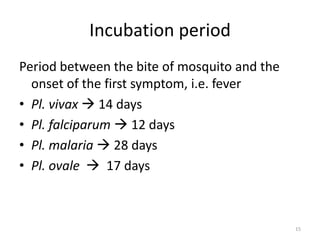
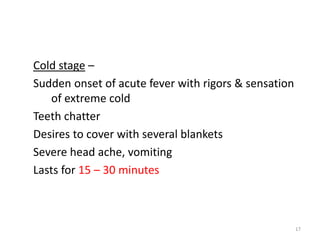
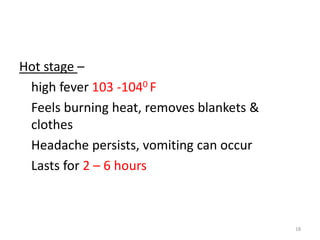
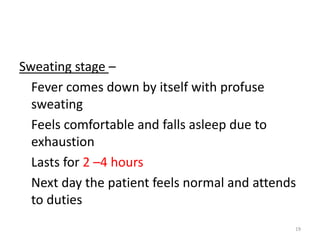
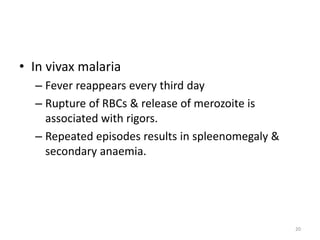
Malaria is caused by a protozoan parasite called Plasmodium, which is transmitted via the bites of infected female Anopheles mosquitoes. The most common symptoms are fever, chills, and sweating that occurs in intermittent periodic cycles. Left untreated, malaria can cause anemia and enlargement of the spleen. There are four types of malaria parasites that can infect humans, with Plasmodium vivax and Plasmodium falciparum being the most prevalent. Malaria is prevalent in tropical and subtropical regions and is controlled through measures that eliminate the parasite reservoir in humans, interrupt mosquito-borne transmission, and protect susceptible individuals.