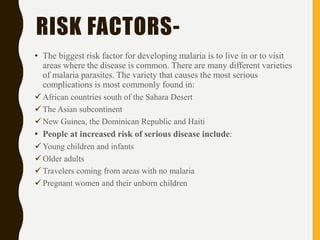
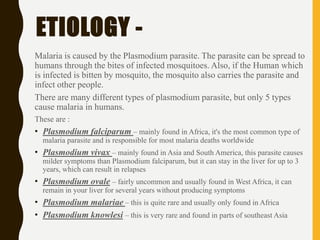
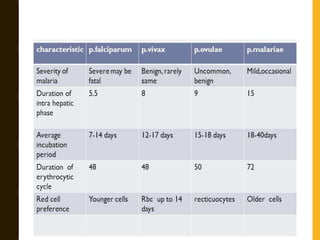
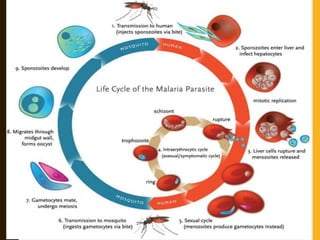
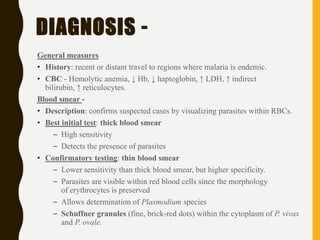
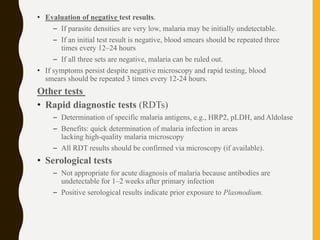
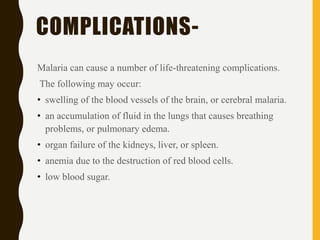
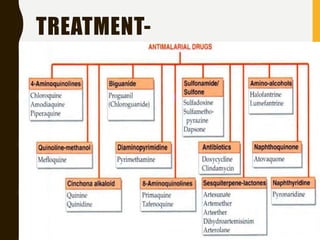
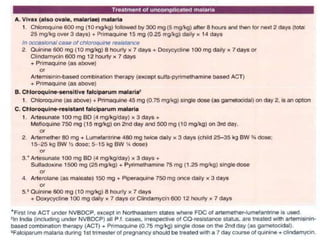
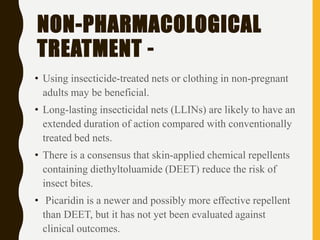
Malaria is an infectious disease caused by protozoan parasites from the Plasmodium family, transmitted through Anopheles mosquito bites, with Plasmodium vivax and Plasmodium falciparum being the most common and deadly species, respectively. It primarily affects tropical regions, leading to significant mortality, particularly in children under five and pregnant women. Diagnosis typically involves blood smears, with treatment focusing on prevention through insect repellent and mosquito nets, as well as pharmacological intervention to eliminate the parasite.