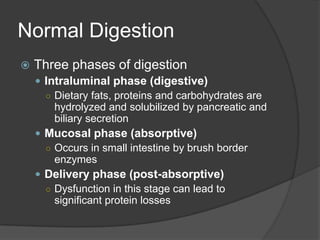
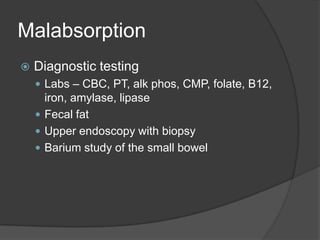
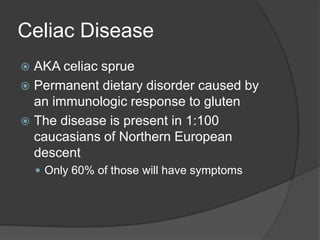
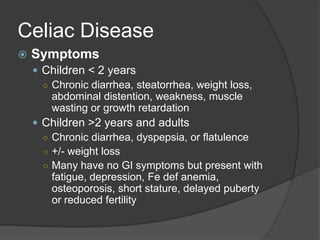
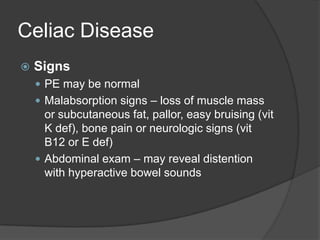
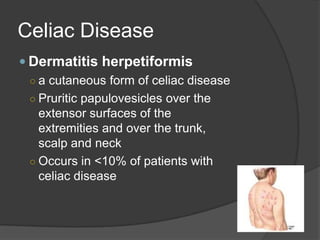
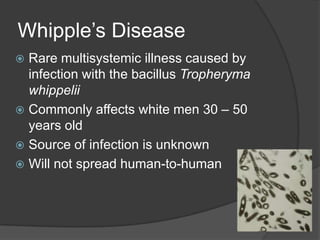
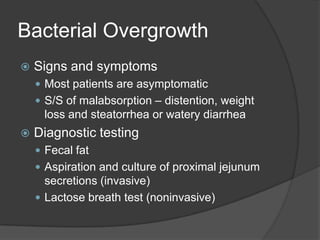
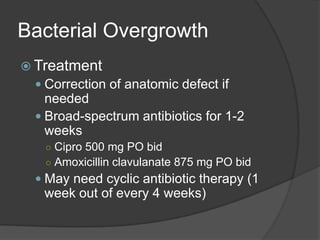
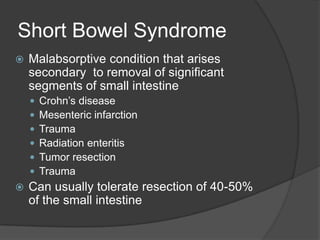
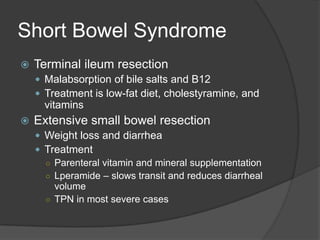
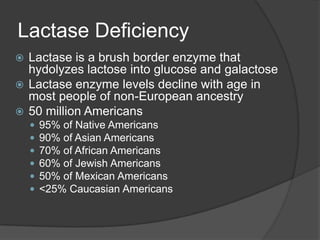
Malabsorption occurs when there is a disruption in the normal digestion and absorption of nutrients in the small intestine. It can cause symptoms like diarrhea, weight loss, and malnutrition. There are several potential causes of malabsorption, including celiac disease, Whipple's disease, bacterial overgrowth, short bowel syndrome, and lactase deficiency. Celiac disease is an immune-mediated reaction to gluten that damages the small intestine and is treated with a gluten-free diet. Whipple's disease is a rare infection caused by Tropheryma whippelii that presents with weight loss and joint pain and is treated with long-term antibiotics. Bacterial overgrowth in the small intestine can also interfere with absorption