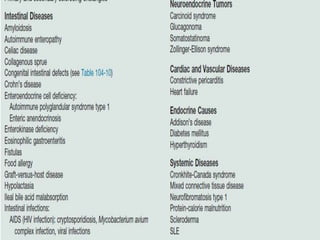
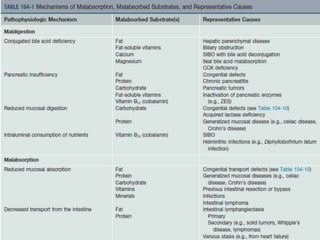
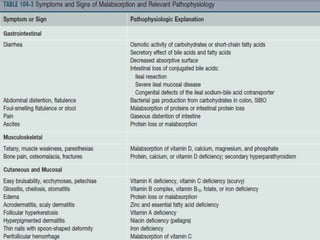
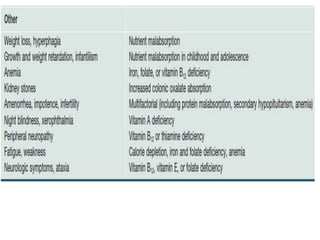
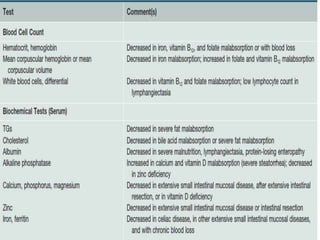
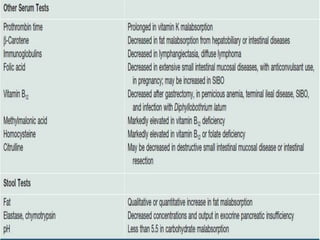
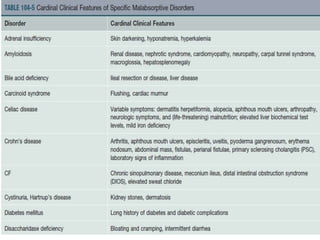
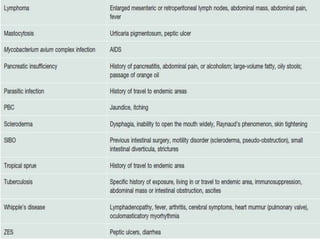
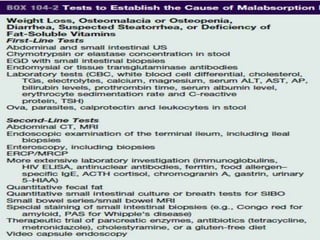
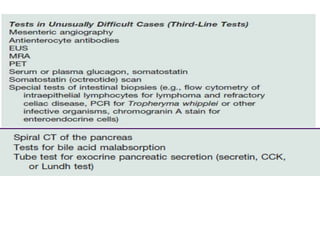
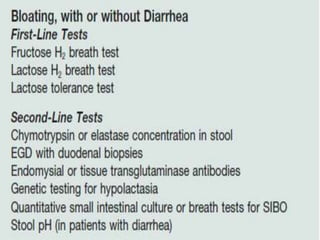
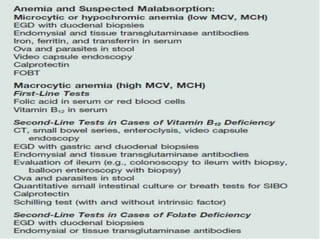
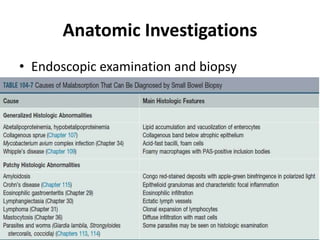
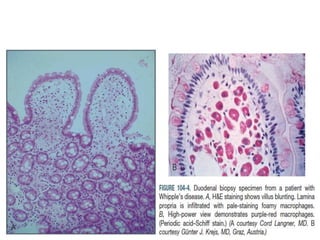
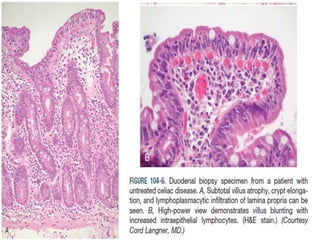
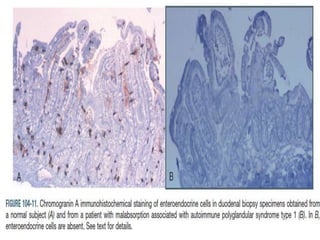
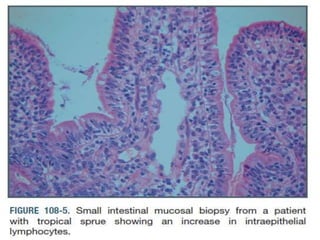
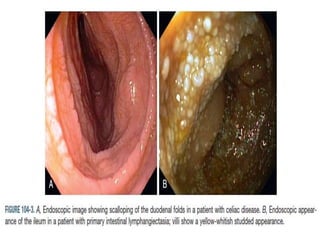
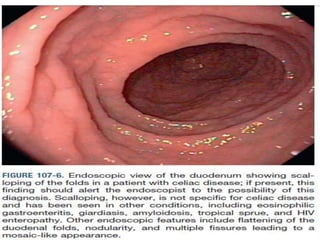
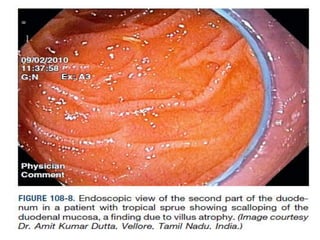
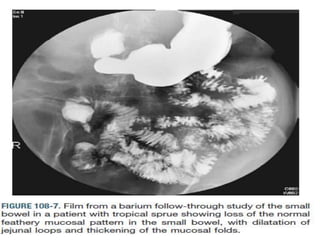
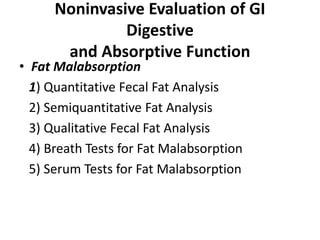
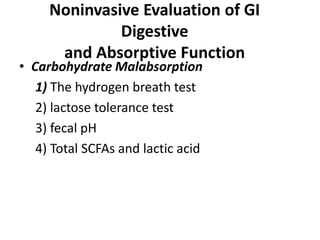
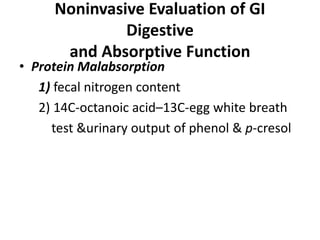
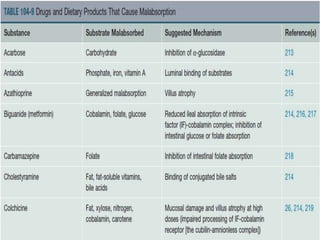
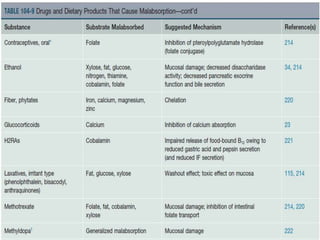
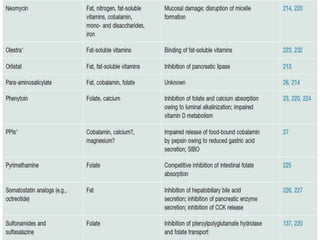
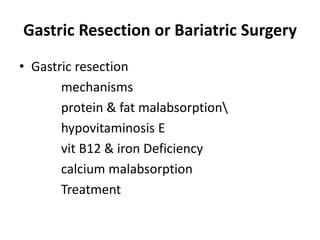
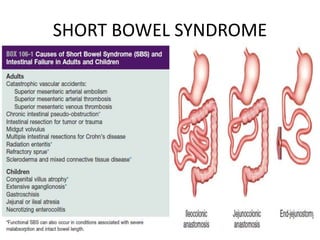
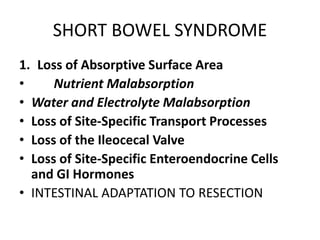
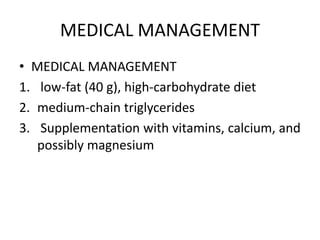
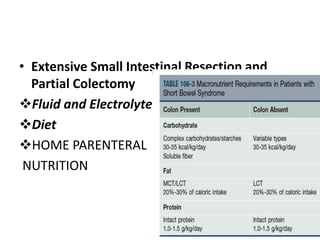
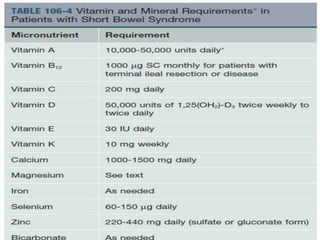
This document provides an overview of approaches to evaluating and managing malabsorption syndromes. It discusses the etiology, pathophysiology, clinical features, diagnostic testing and general management strategies for a wide range of conditions that can cause malabsorption including celiac disease, short bowel syndrome, exocrine pancreatic insufficiency, bile acid malabsorption, infections, surgeries, and other disorders. The evaluation involves a detailed history, physical exam, initial lab tests, and may require endoscopic examination, imaging, and specialized tests of digestive and absorptive functions. Management is directed at the underlying cause, correcting nutritional deficiencies, and addressing symptoms.