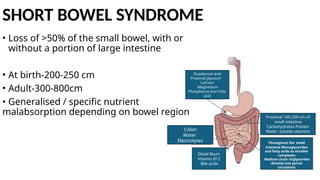
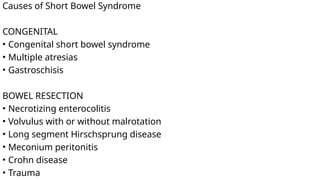
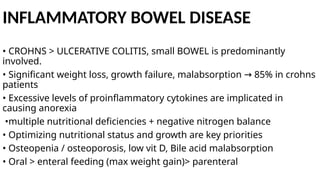
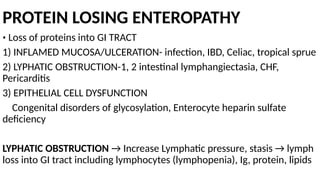
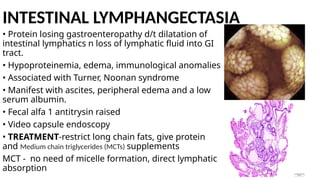
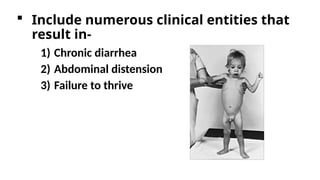
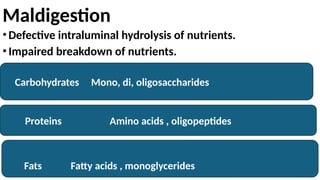
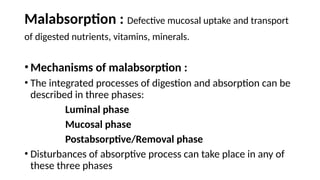
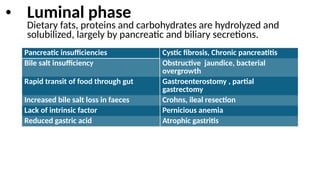
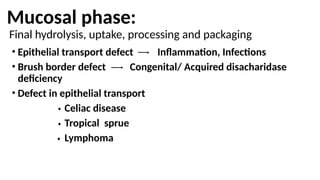
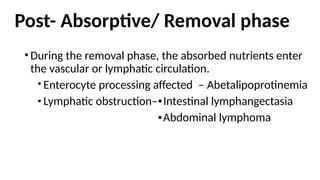
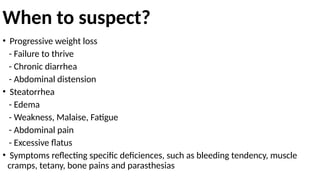
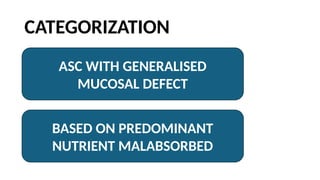
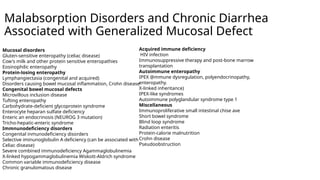
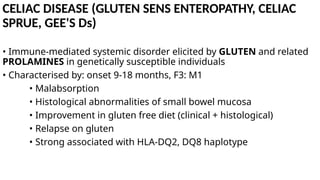
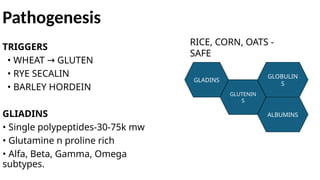
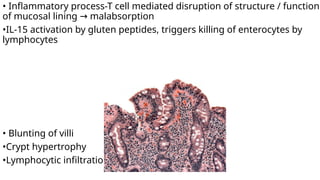
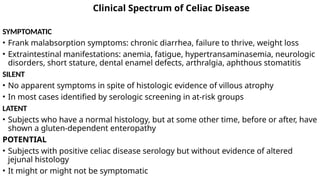
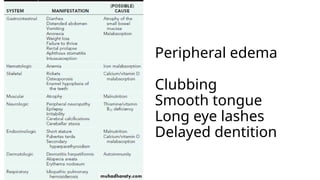
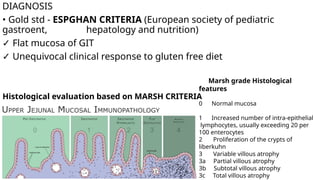
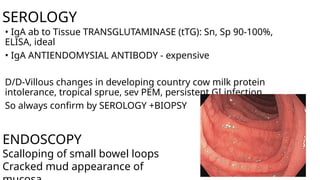
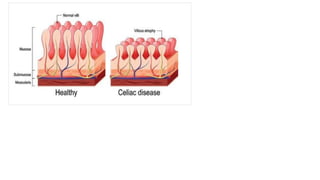
The document discusses malabsorption in children, detailing its clinical entities, symptoms, and various underlying mechanisms affecting digestion and absorption. It highlights the different phases of nutrient processing, potential causes such as infections and diseases, and specific nutrient deficiencies, with an emphasis on conditions like celiac disease and tropical sprue. Additionally, it covers diagnostic methods, treatment options, and the significance of a gluten-free diet for managing malabsorption disorders.
![• BLOOD: LOW levels of B12, A, E, D, K, folate, calcium
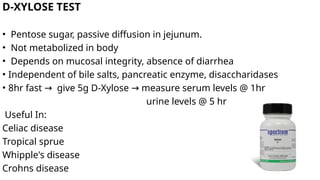
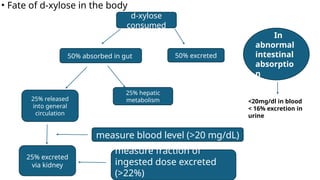
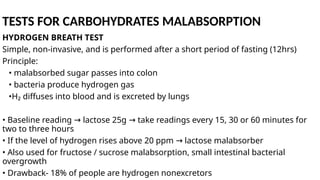
•D-XYLOSE test is positive
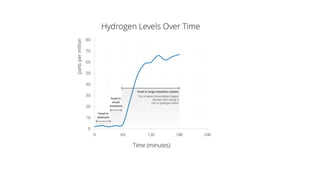
• Stearorrhea in 90% H2 breath test - POSITIVE (d/t bacterial
overgrowth)
• Barium meal - thickened small bowel
• Biopsy - thick basement membrane, triglyceride accumulation near to
surface epithelium [celiac - lipid droplets in enterocyte]
• Injury to entire small bowel (not proximal as in celiac sprue)
• No changes with GLUTEN FREE DIET
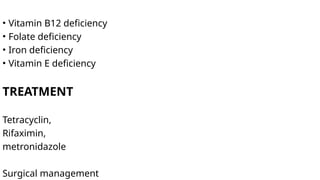
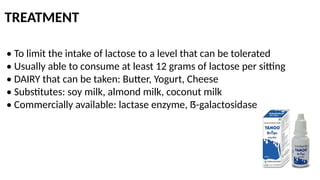
TREATMENT
• TETRACYCLINE/CO-TRIMOXAZOLE for 3-6months
• Deficiency correction-B12, folic acid](https://image.slidesharecdn.com/presentation5-241004052116-5d207672/85/MALABSORPTION-SYNDROMES-IN-PEDIATRICS-POPULATION-27-320.jpg)