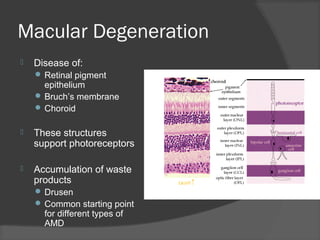
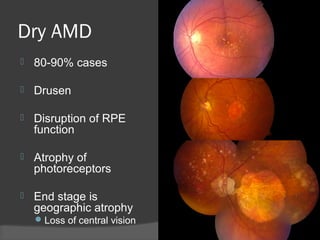
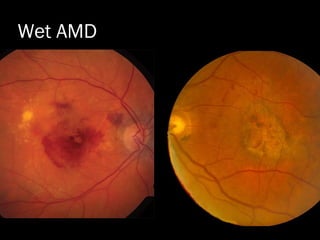
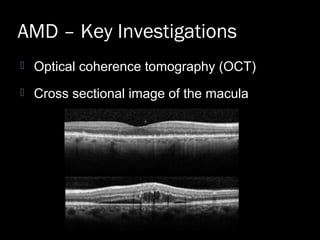
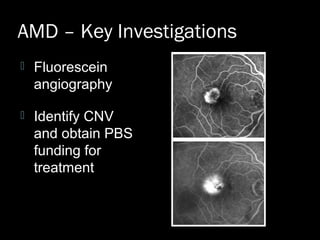
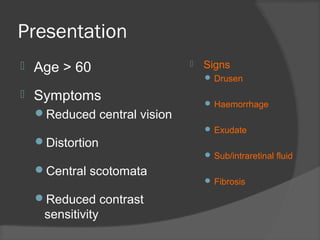
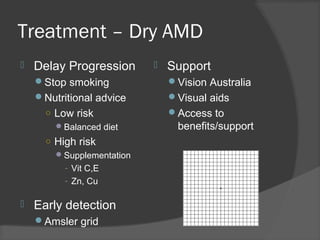
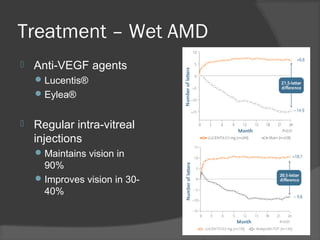
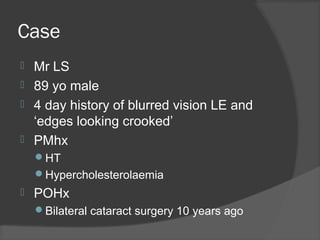
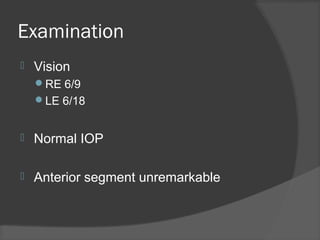
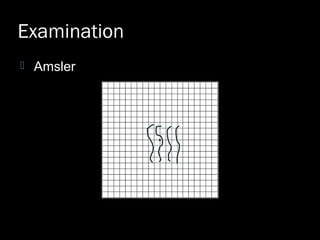
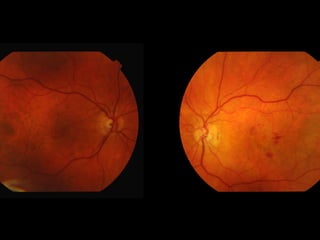
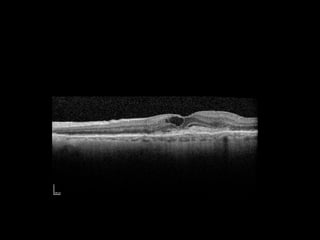
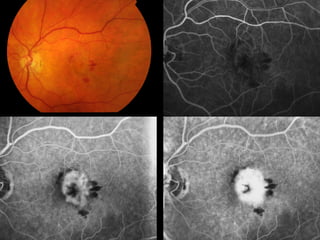
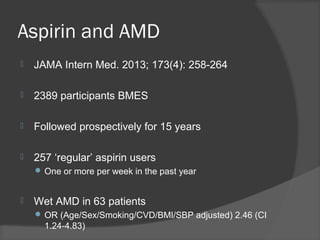
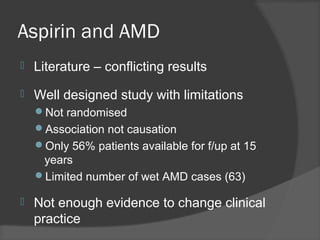
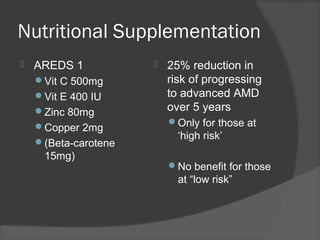
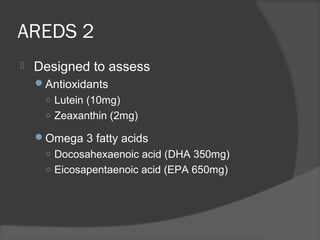
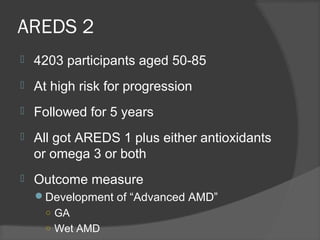
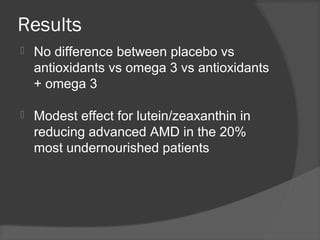
This document discusses macular degeneration (AMD), including its causes, types (dry and wet), investigations like OCT and fluorescein angiography, symptoms, signs, and treatments. It notes that dry AMD accounts for 80-90% of cases and involves drusen and retinal pigment epithelium changes, while wet AMD involves choroidal neovascularization, leakage, and vision loss. Treatments discussed include nutritional supplementation based on AREDS trials, regular anti-VEGF injections for wet AMD, and monitoring for dry AMD.