Embed presentation
Downloaded 27 times

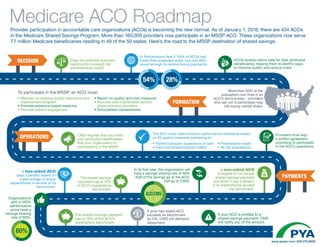
The document discusses the operations and financial implications for Accountable Care Organizations (ACOs) participating in the Medicare Shared Savings Program (MSSP). It highlights that while 54% of ACOs had lower-than-projected costs, only 28% received bonus payments, and emphasizes the importance of quality assurance, patient engagement, and care coordination. As of January 1, 2016, there are 434 ACOs serving 7.7 million Medicare beneficiaries, with a structured approach for shared savings and penalties based on performance metrics.