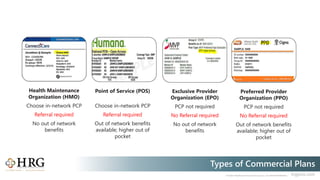
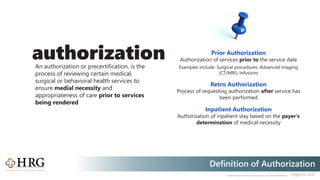
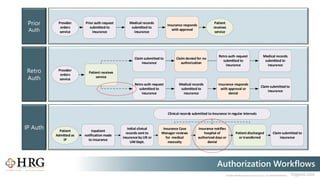
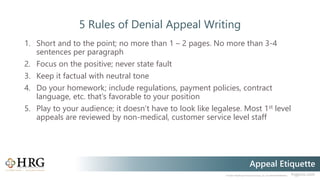
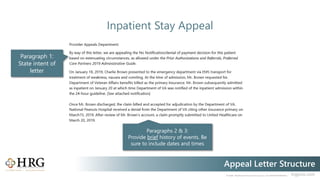
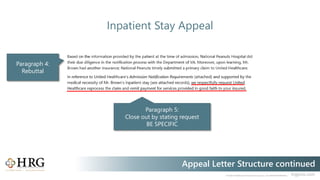
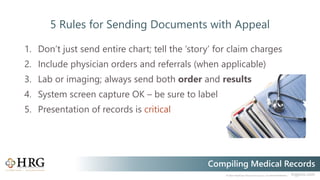
The document outlines the differences between referrals and authorizations in healthcare, detailing various insurance plans that require these processes. It also provides guidance on authorization workflows, effective appeal writing for denied claims, and tips for compiling medical records for submissions. Overall, it serves as a resource for navigating insurance requirements in medical procedures.