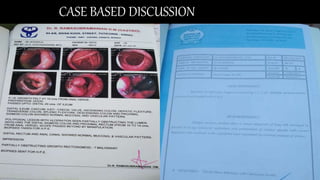
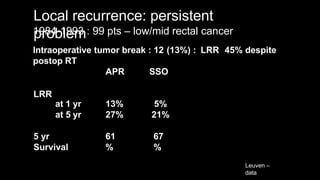
- The patient is a 36-year-old man who underwent neoadjuvant chemoradiotherapy in 2015 for rectal cancer.
- In 2021, he presented with frequent urination. Imaging showed a large recurrent mass involving abdominal structures.
- Biopsy of the skin deposit was suspicious for metastatic mucinous carcinoma.
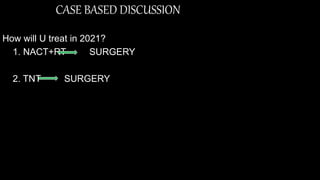
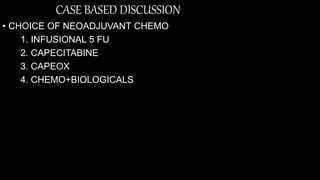
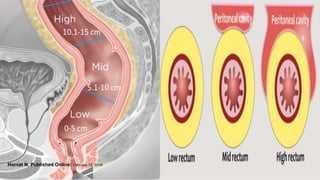
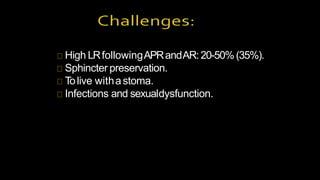
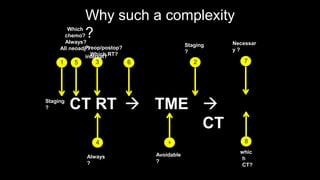
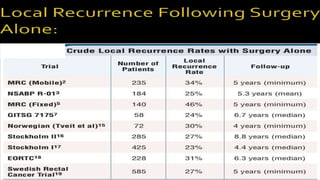
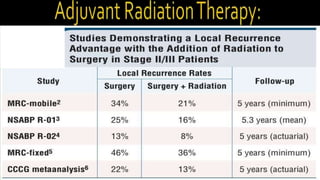
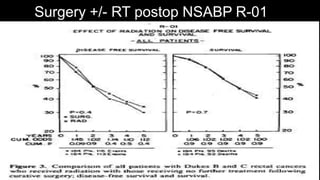
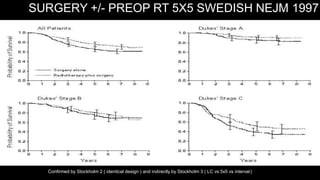
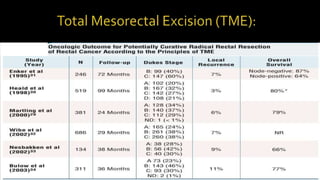
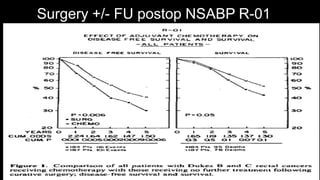
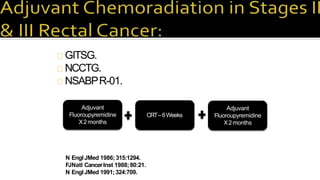
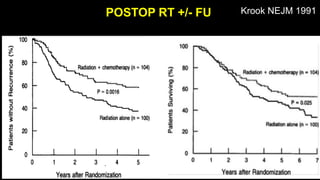
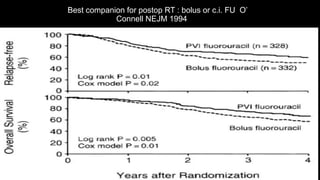
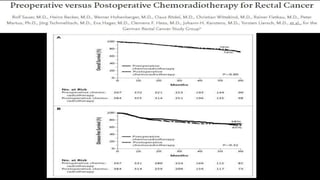
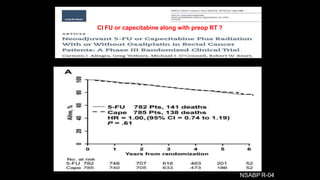
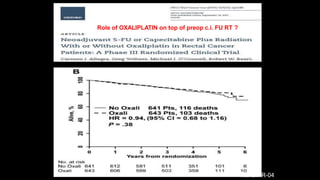
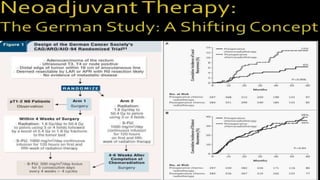
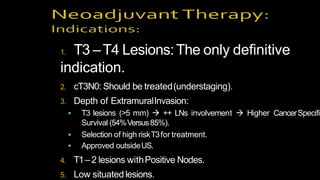
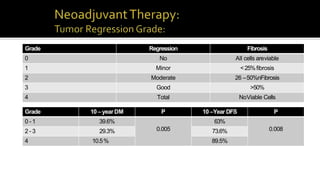
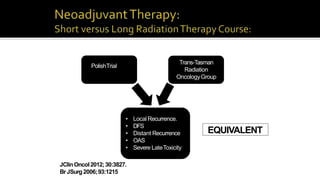
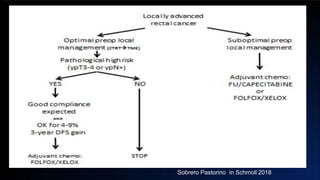
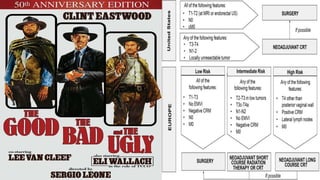
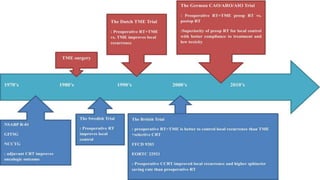
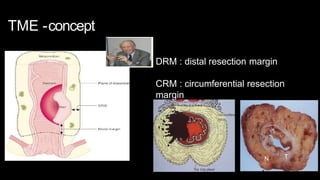
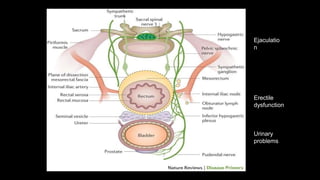
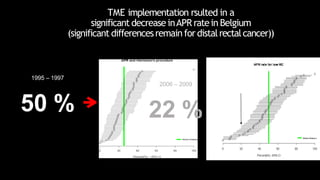
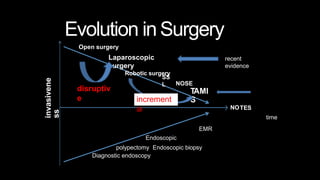
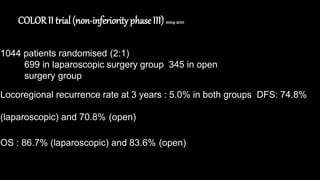
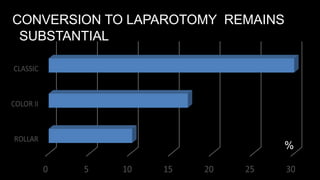
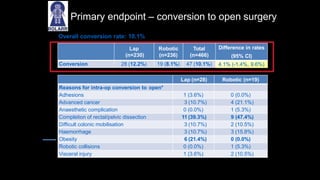
- The case discusses the current treatment approaches for locally advanced rectal cancer, including neoadjuvant and total neoadjuvant therapy options, and choices for chemotherapy and radiotherapy.