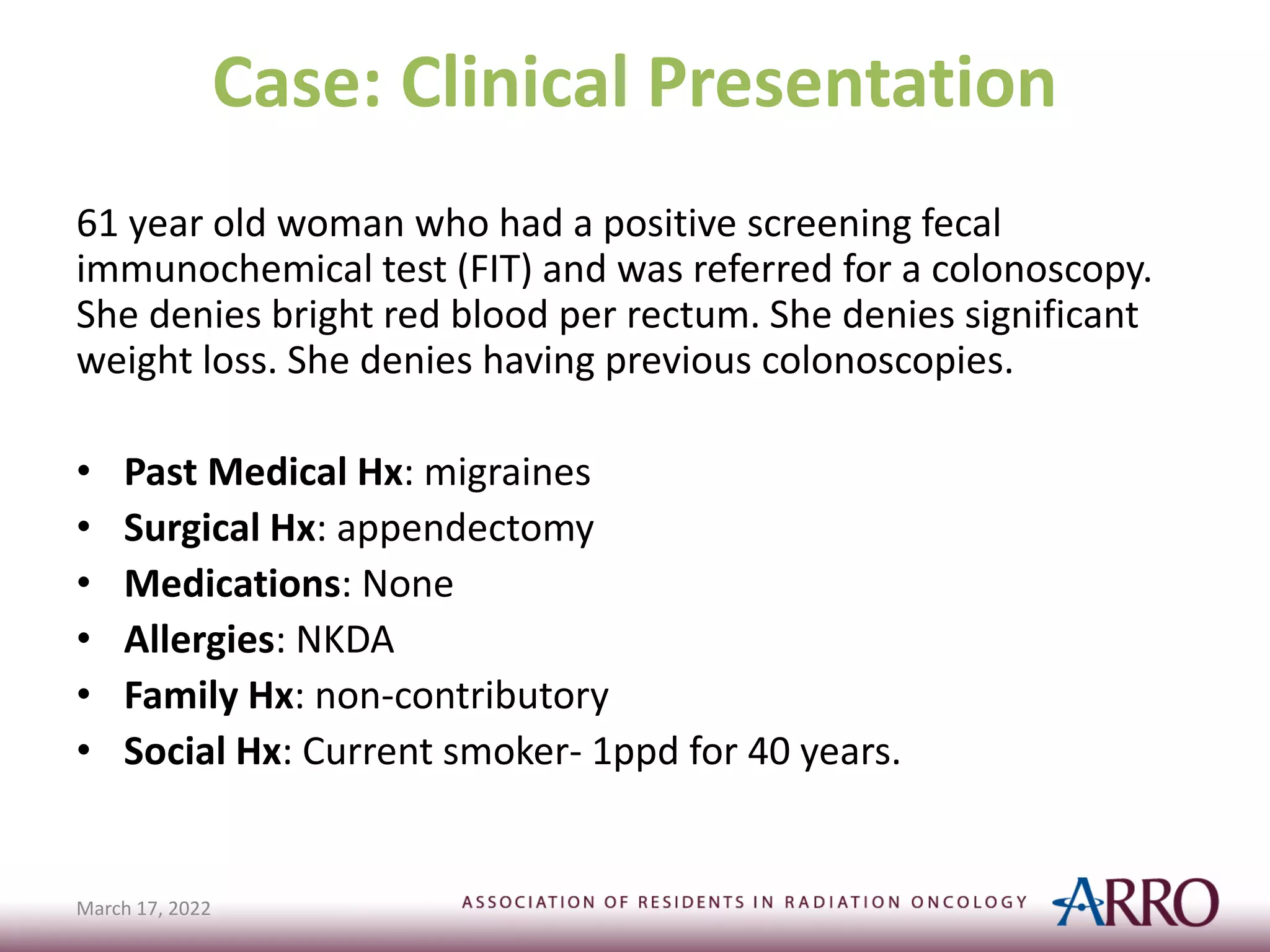
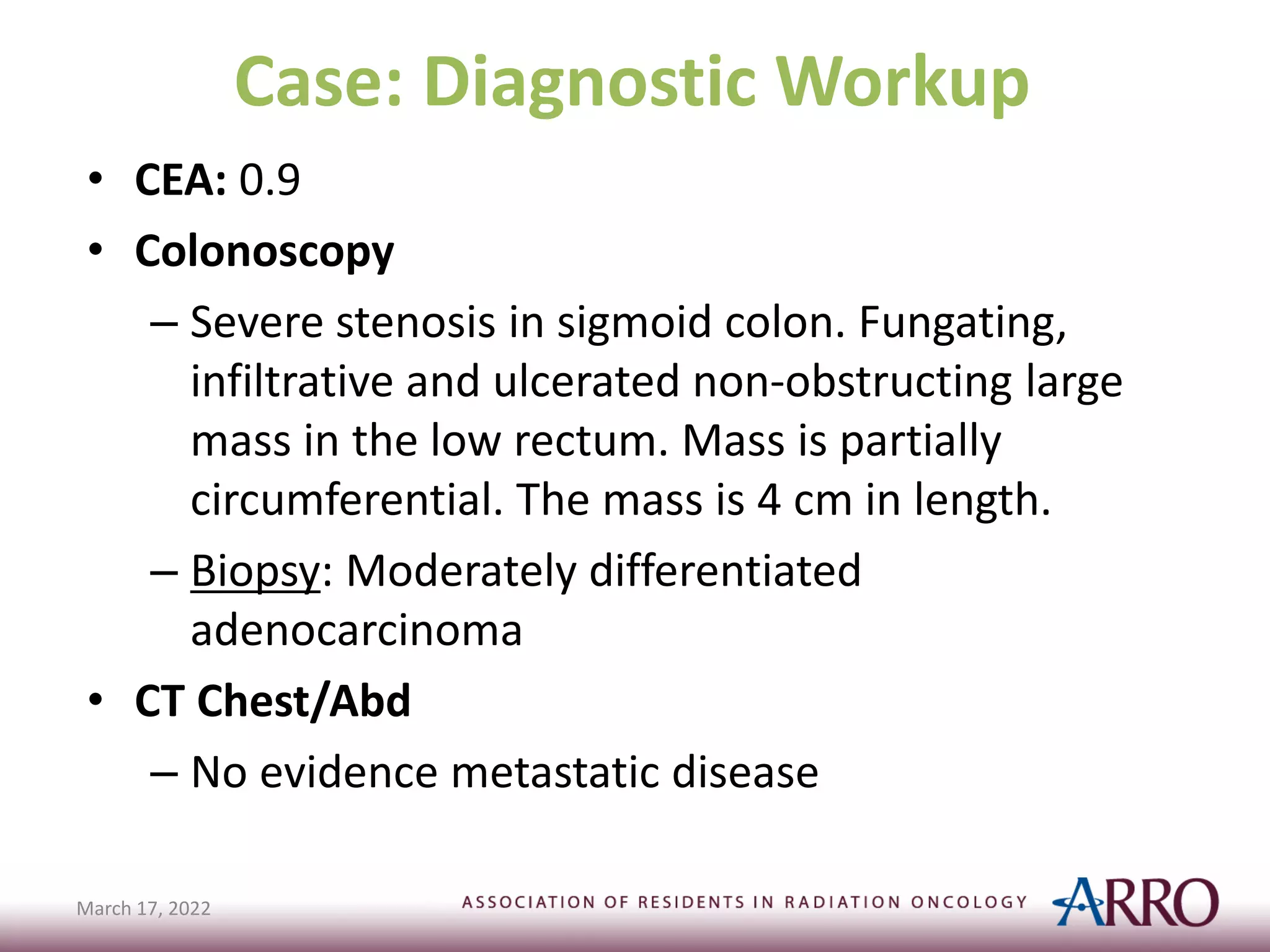
This document discusses the management of rectal cancer in a 61-year-old woman. It was found that she has a cT4bN2b rectal adenocarcinoma. After discussion, the decision was made to proceed with total neoadjuvant therapy consisting of chemoradiation followed by chemotherapy and then surgery. The patient tolerated treatment well with no residual toxicities after chemoradiation. She will proceed with resection after completing chemotherapy.















![Workup
• H&P
– DRE – evaluate sphincter function (predictor of subsequent
continence)
• Rigid Proctoscopy – assess primary tumor and biopsy
• Colonoscopy – detect possible synchronous primaries
• CT chest, abdomen, and pelvis – detect metastatic disease
• Endorectal ultrasound (ERUS) – accurate in predicting T category,
assess depth of tumor penetration and adjacent mesorectal and
pelvic LNs
• MRI – accurate in predicting T-category and mesorectal fascial
involvement (circumferential resection margin [CRM] positivity),
assess involvement of LNs based on size criteria
• PET – helpful for LN involvement when indicated
• CBC, CEA
March 17, 2022](https://image.slidesharecdn.com/arrocaserectaldefinitivemanagement-230615121429-ec613f9c/75/ARROCase_Rectal_DefinitiveManagement-pdf-18-2048.jpg)