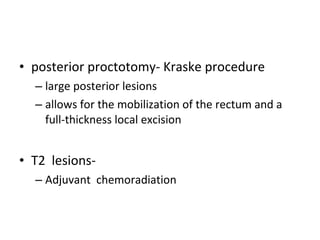
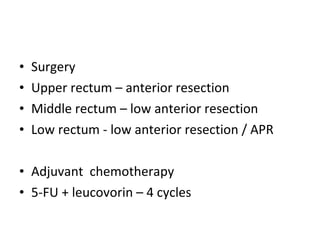
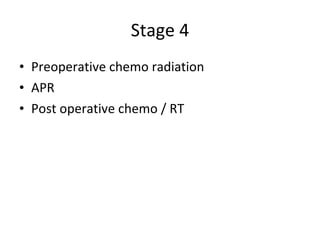
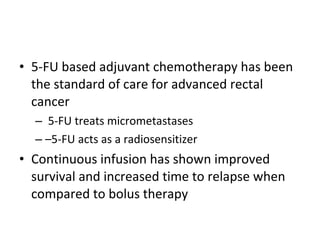
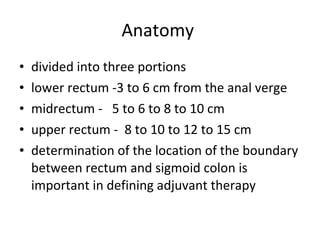
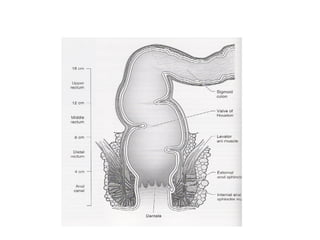
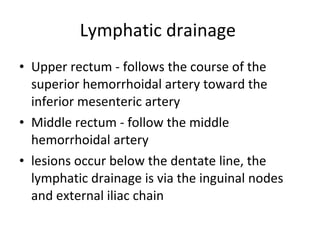
Carcinoma rectum has several risk factors including family history, inflammatory bowel disease, and genetic conditions. The rectum is divided into three portions with different lymphatic drainage patterns and implications for surgery. Staging includes Dukes', Astler-Coller, TNM, and clinical features are important for diagnosis. Treatment depends on stage and may include transanal excision, chemoradiation, surgery such as anterior resection or APR, and adjuvant therapy.









![TNM staging TX- Primary tumor cannot be assessed T0 - No evidence of primary tumor Tis - Carcinoma in situ: intraepithelial or invasion of lamina propria [*] T1 - Tumor invades submucosa T2 - Tumor invades muscularis propria T3- Tumor invades through the muscularis propria into the subserosa, or into nonperitonealized pericolic or perirectal tissues T4 Tumor directly invades other organs or structures and/or perforates visceral peritoneum [†]](https://image.slidesharecdn.com/carcinomarectum-110220041034-phpapp02/85/Carcinoma-rectum-14-320.jpg)

![STAGE T N M DUKES [§] MAC [§] 0 Tis N0 M0 I T1 N0 M0 A A T2 N0 M0 A B1 IIA T3 N0 M0 B B2 IIB T4 N0 M0 B B3 IIIA T1-T2 N1 M0 C C1 IIIB T3-T4 N1 M0 C C2 IIIC Any T N2 M0 C C1/C2 IV Any T Any N M1 D](https://image.slidesharecdn.com/carcinomarectum-110220041034-phpapp02/85/Carcinoma-rectum-17-320.jpg)