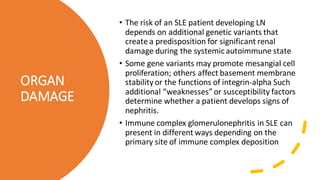
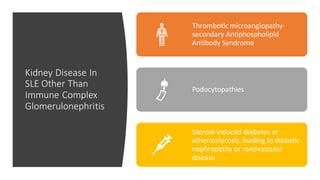
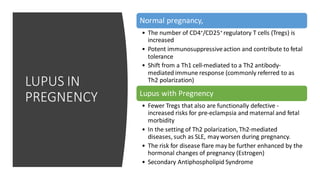
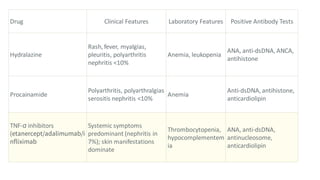
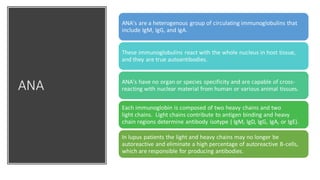
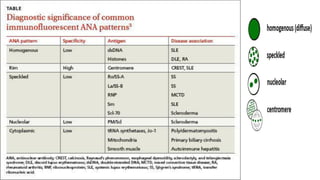
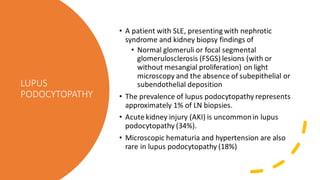
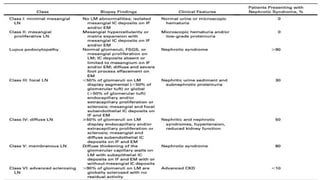
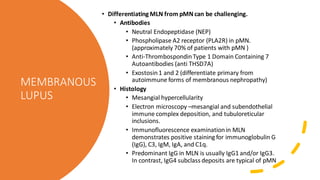
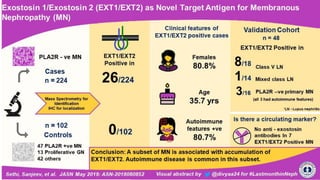
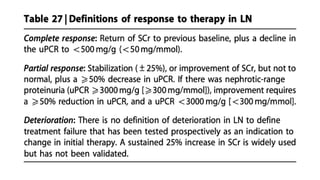
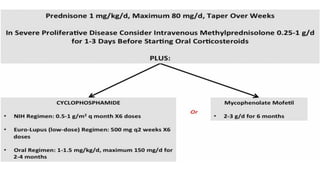
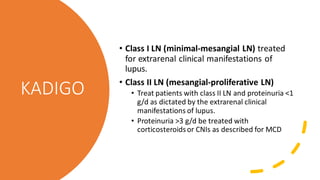
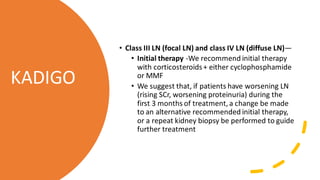
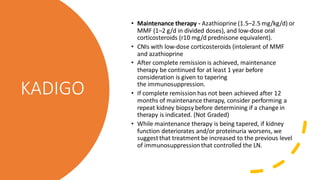
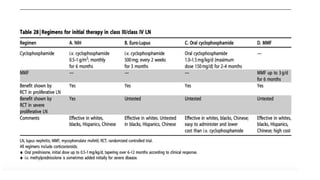
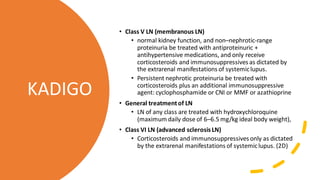
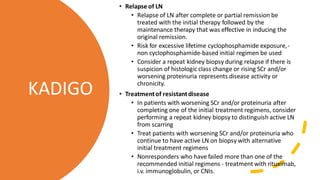
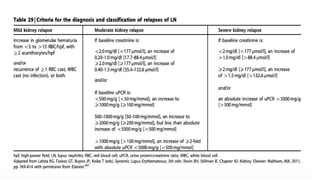
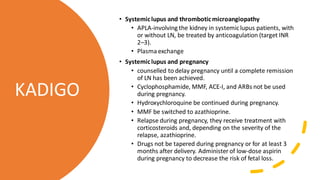
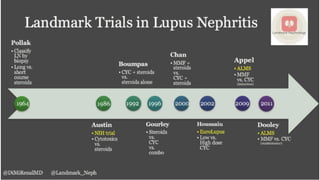
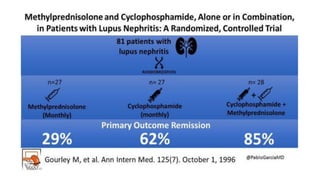
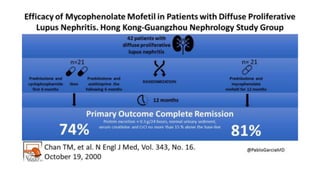
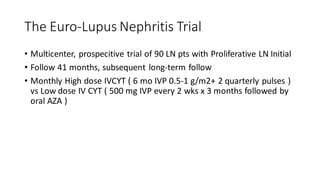
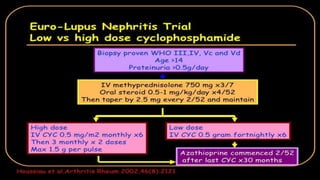
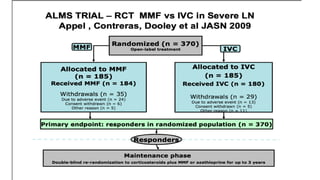
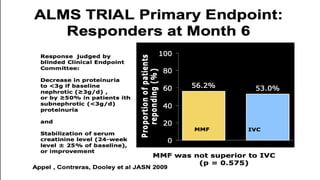
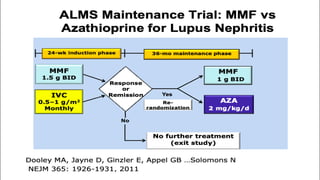
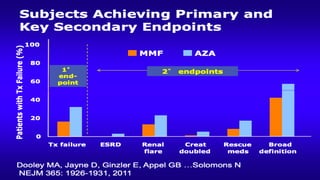
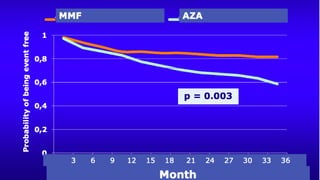
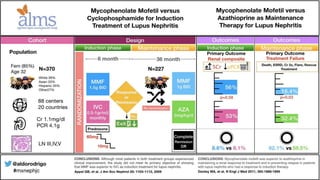
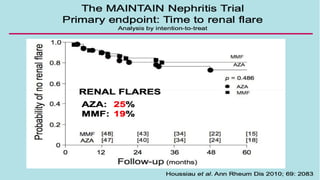
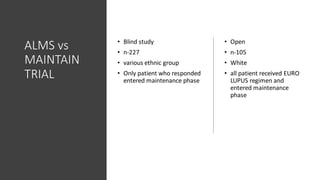
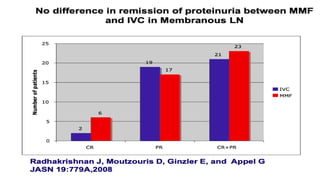
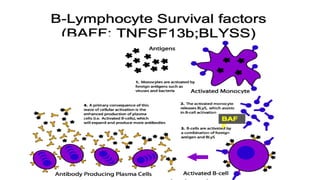
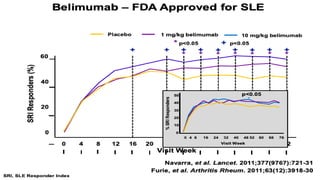
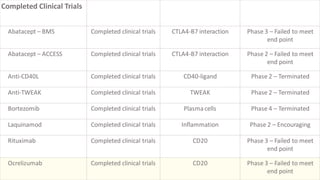
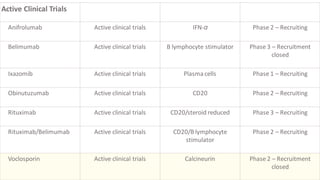
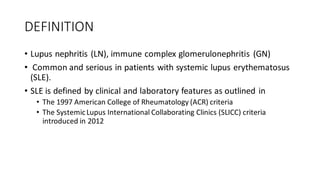
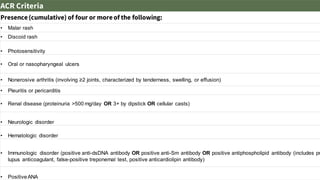
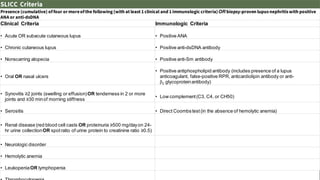
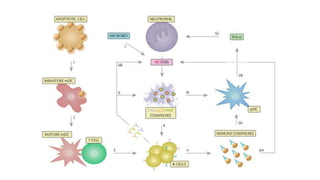
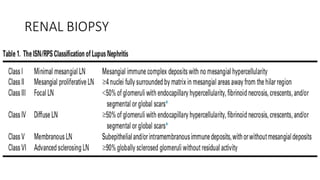
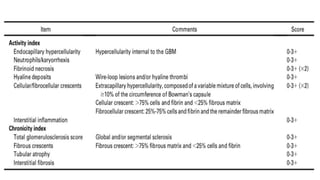
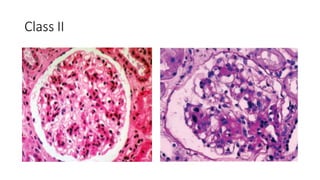
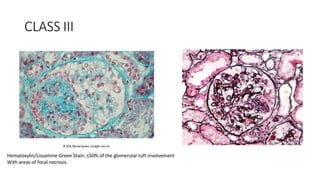
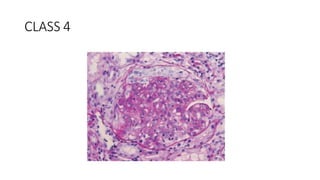
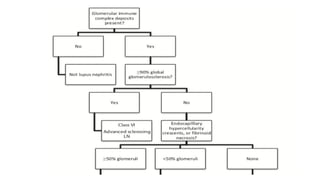
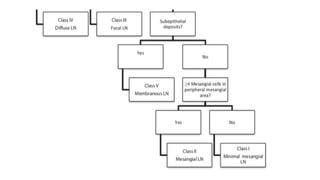
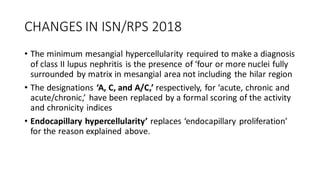
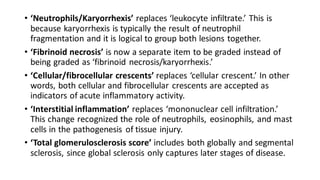
The document discusses the pathogenesis of lupus nephritis, including the loss of immune tolerance leading to autovaccination and persistent antinuclear antibodies, with a subset of patients developing lupus nephritis depending on additional genetic susceptibility factors; it also covers the classification, treatment approaches including immunosuppressive therapies, and clinical trials of lupus nephritis.