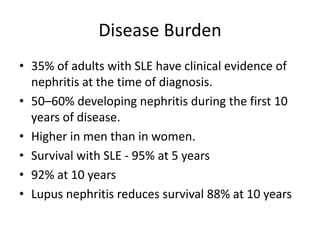
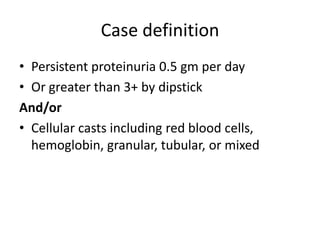
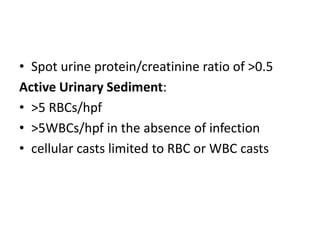
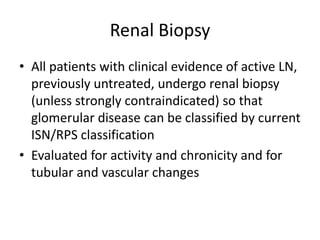
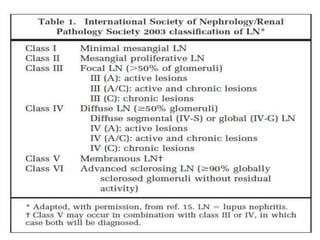
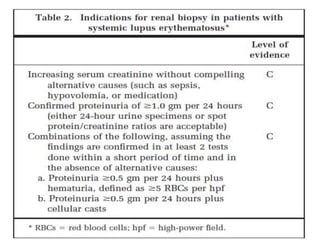
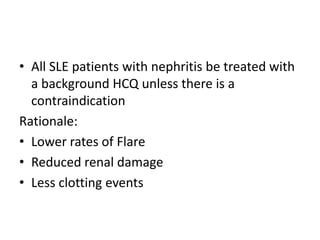
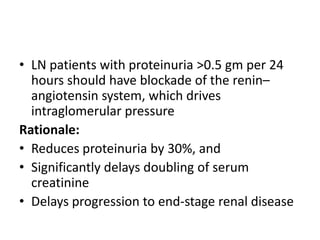
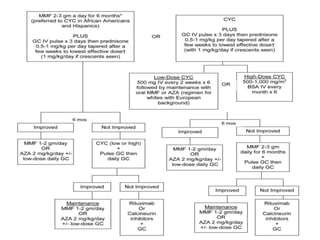
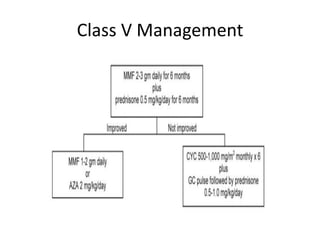
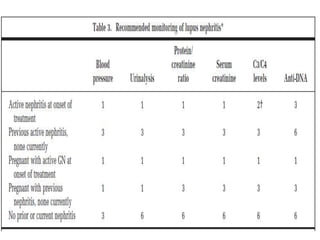
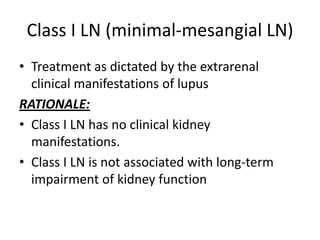
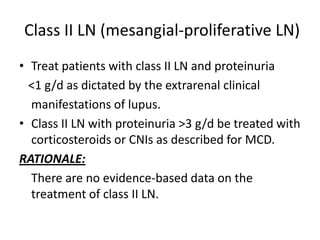
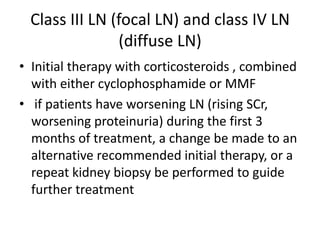
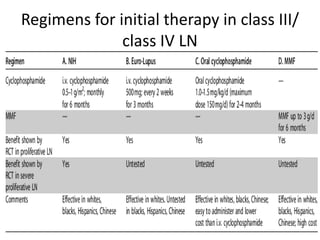
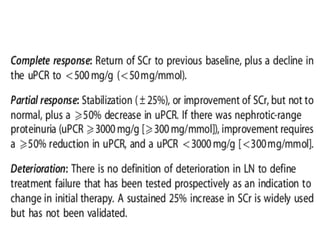
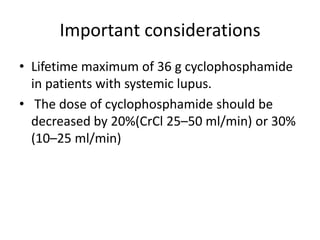
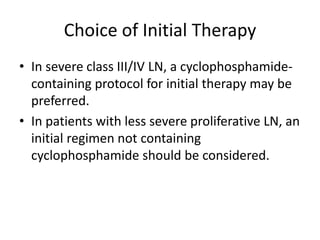
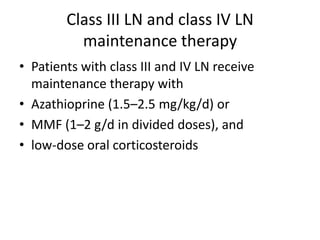
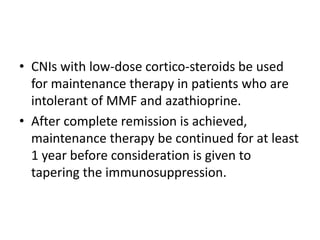
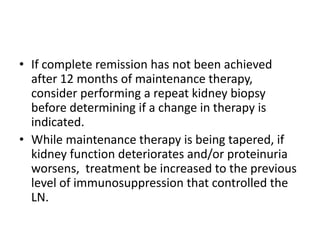
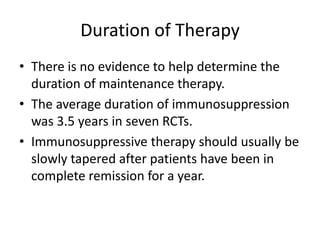
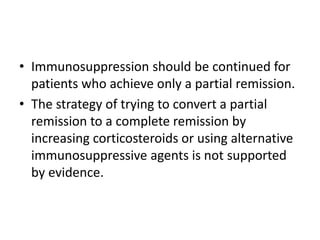
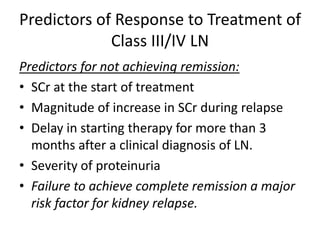
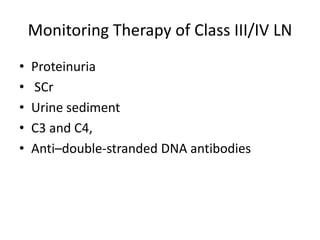
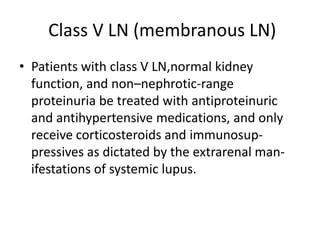
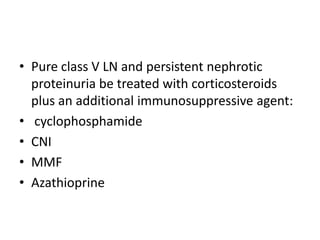
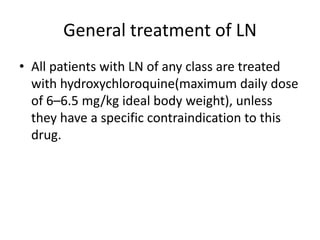
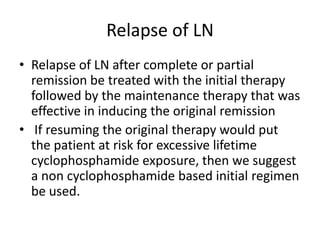
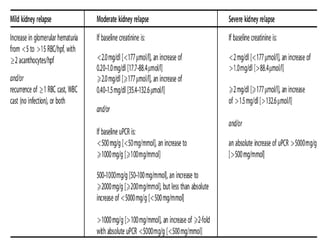
This document provides guidelines for screening, treating, and managing lupus nephritis (LN). It defines LN and its classification system. For classes I and II LN, treatment focuses on extrarenal symptoms. Classes III and IV are treated aggressively with glucocorticoids and immunosuppressants. Maintenance therapy includes azathioprine or mycophenolate mofetil with low-dose steroids. Relapse is treated with the initial regimen. The guidelines recommend treatments and monitoring for various LN classes and complications.