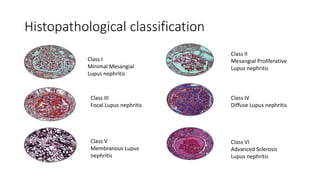
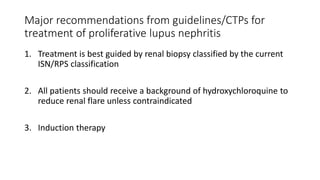
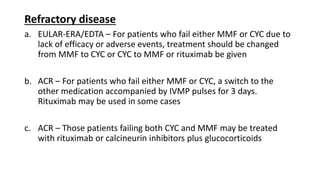
The document discusses the management of systemic lupus erythematosus (SLE) and lupus nephritis, including treatment approaches, monitoring patients, addressing neuropsychiatric involvement, managing pregnancy in SLE patients, and approaches to babies born to mothers with SLE. It provides details on disease classification, induction and maintenance therapies, treatment response criteria, and recommendations from clinical practice guidelines.