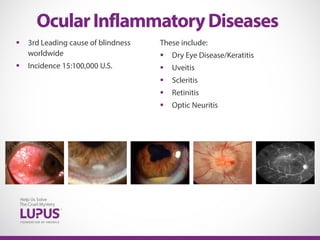
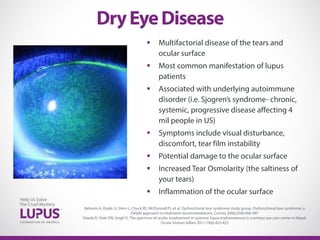
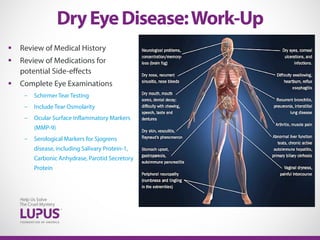
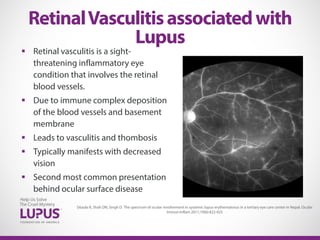
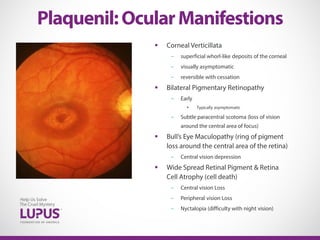
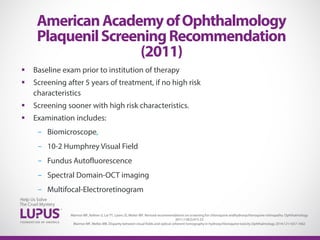
The document discusses the ocular complications associated with lupus, emphasizing that lupus is a leading cause of blindness globally and can lead to various eye conditions such as dry eye disease, uveitis, and retinal vasculitis. It highlights the significance of thorough eye examinations and appropriate treatments, including the management of dry eye and monitoring for potential side effects of lupus medications like hydroxychloroquine. Comprehensive screening recommendations for monitoring retinal toxicity and long-term effects are also detailed.