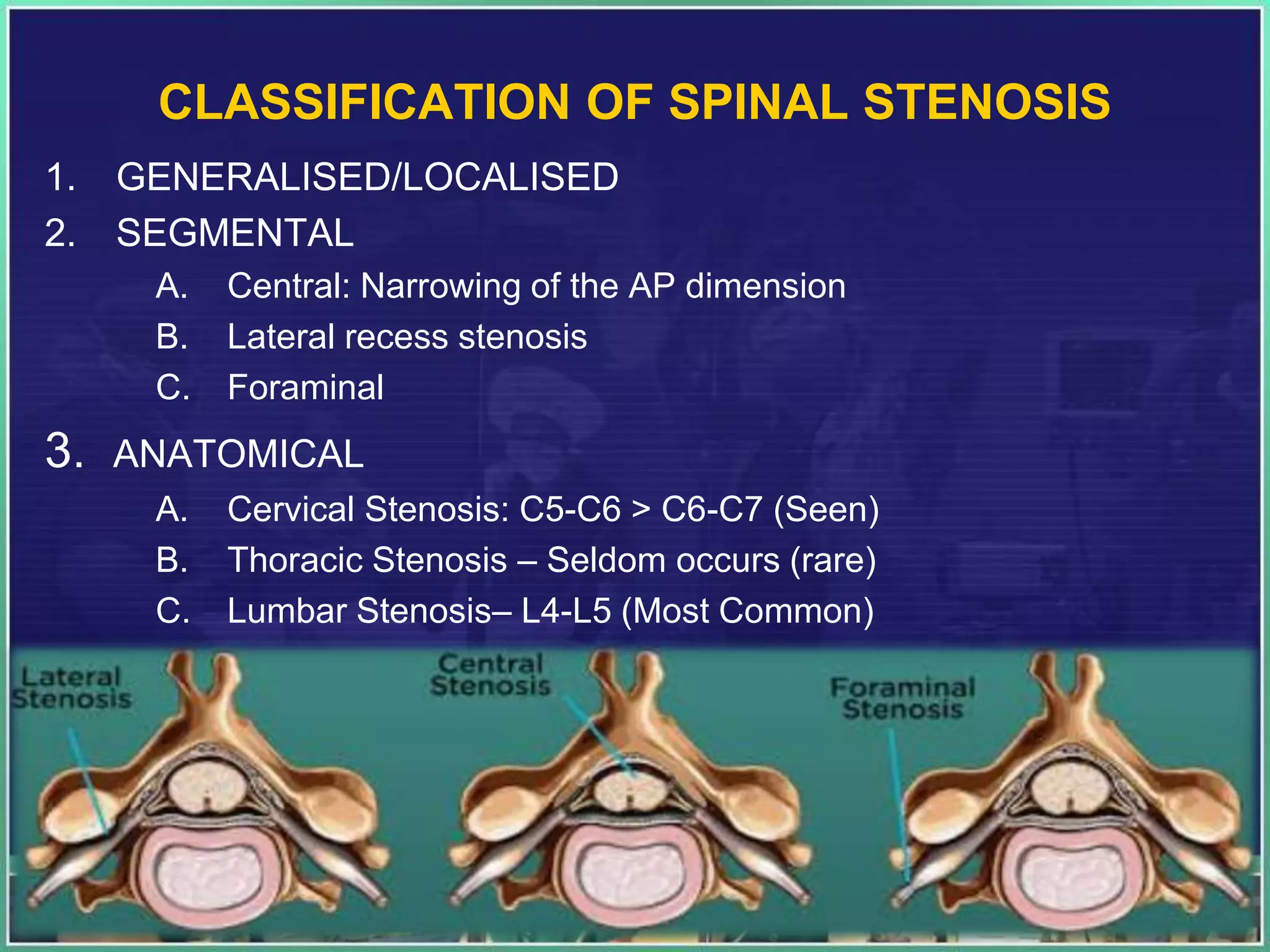
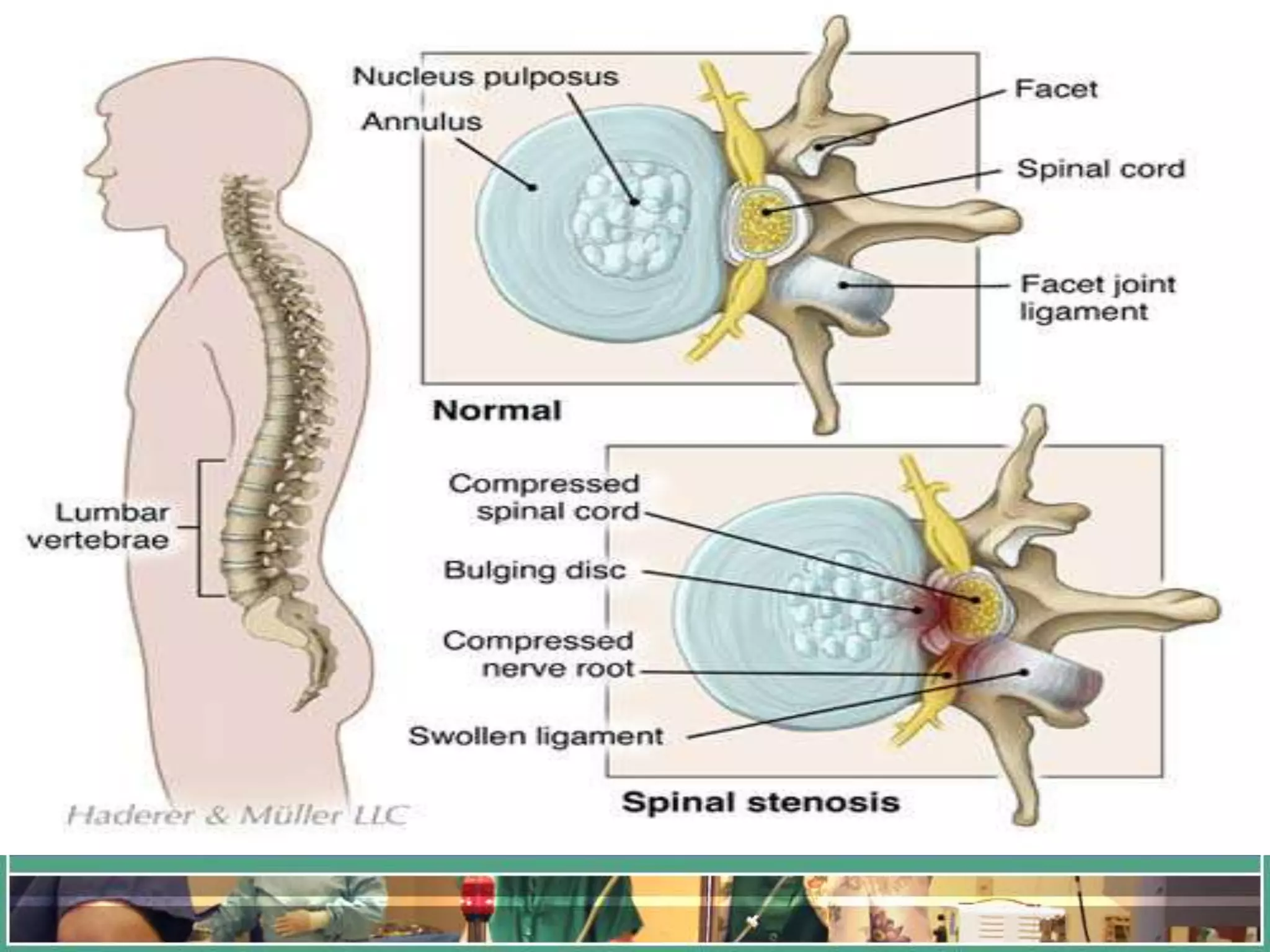
Lumbar spinal stenosis is a narrowing of the spinal canal in the lower back that puts pressure on the spinal cord and nerves. It commonly occurs in people over 50 due to age-related wear and tear causing bone spurs or thickened ligaments. The best test for diagnosis is an MRI of the lumbar spine, which will show if there is compression of the spinal cord or nerves. Conservative treatment includes medications like NSAIDs, muscle relaxants, and epidural steroid injections, as well as physical therapy. Surgery such as laminectomy or discectomy may be considered if conservative measures fail to provide relief from pain and symptoms.


























































![High-yield Points
• Spinal -- epidural abscess - Staph. aurous [50 – 60%]
• Cervical Spondylosis: Most common occurs at C5-6 > C6-7 levels
• Sciatica is the most common symptom of a lumbar herniated disc
• Sciatica most commonly caused by lumbar disc prolapse
• Piriformis muscle compression lead to Sciatica/ Sciatica-type-pain
• Whiplash Injury- Hyperextension of lower cervical spin
• Jefferson fracture is burst fracture of ring of atlas (C1) vertebrae
• Burst fracture is a vertical compression fracture
• Flexion rotation injury is the most common spinal injury followed by
compression extension injury (2nd most common).
• Tear drop fracture is caused by combined axial compression and flexion
injury
• Hangman’s Fracture- It occurs when a fracture line passes through the
neural arch of the axis (C2) vertebrae](https://image.slidesharecdn.com/lumbarspinalstenosislaminectomyimp-210404194052/75/Lumbar-spinal-stenosis-laminectomy-prolapsed-intervertebral-disc-65-2048.jpg)


