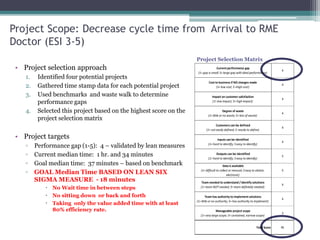
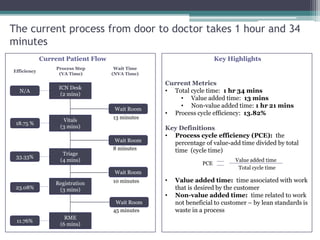
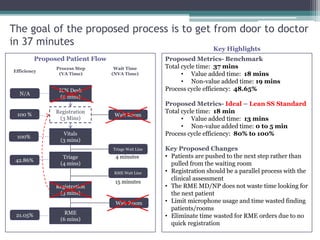
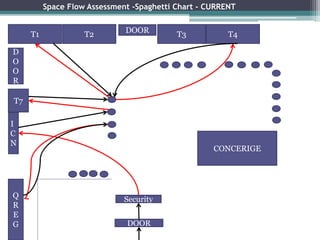
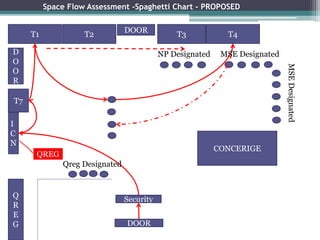
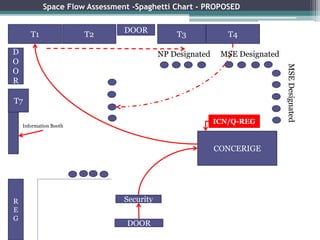
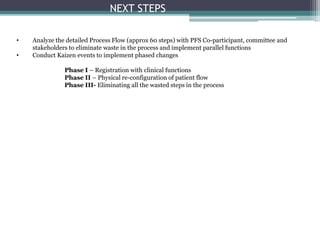
The document summarizes a Lean Six Sigma project to decrease the cycle time from arrival to receiving a medical evaluation (RME) for emergency department patients with an acuity level of 3-5. The current median time is 1 hour and 34 minutes with significant non-value added time. The project aims to reduce the median time to 37 minutes initially and ultimately 18 minutes by streamlining the process and eliminating waste. Key changes proposed include parallel registration and clinical assessment, pushing patients to the next step rather than pulling from waiting rooms, and eliminating unnecessary waiting between steps. Next steps outlined are analyzing the detailed process flow, conducting Kaizen events to implement changes in phases, and ultimately eliminating all wasted steps.