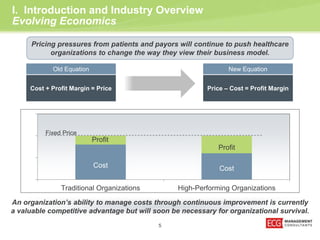
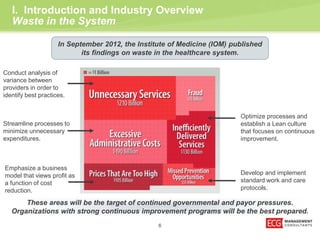
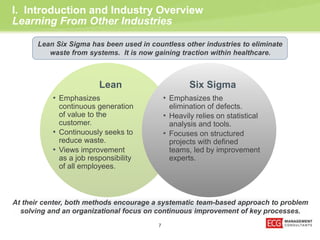
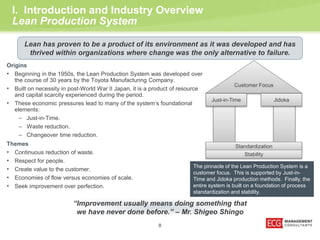
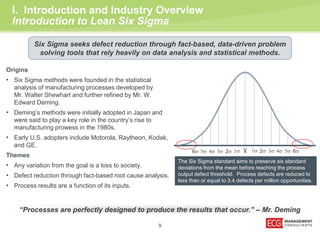
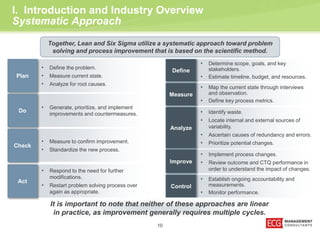
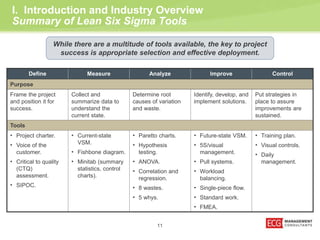
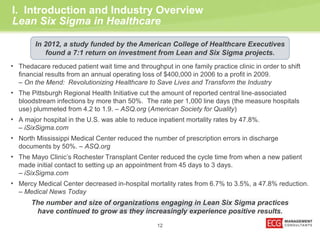
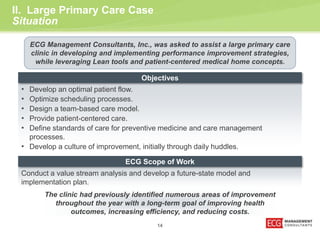
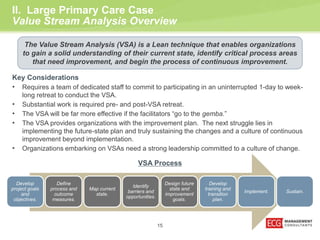
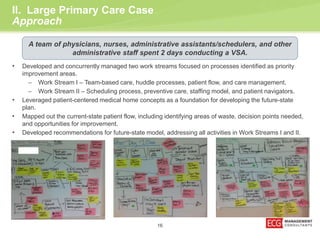
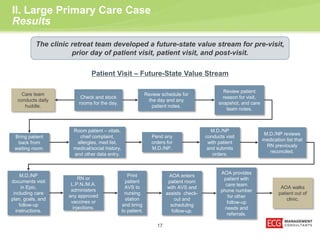
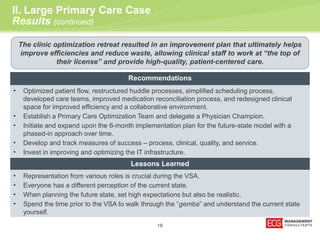
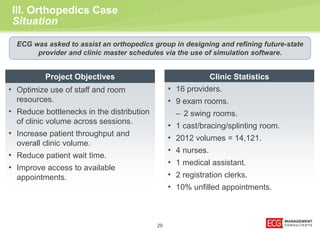
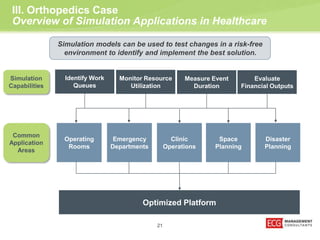
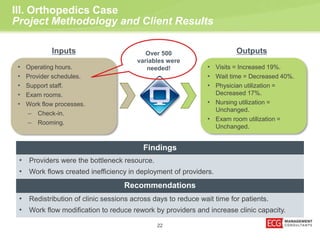
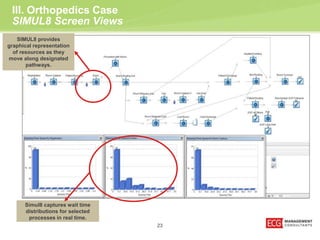
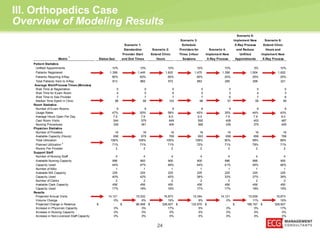
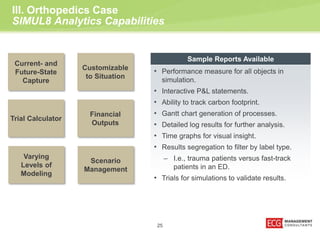
The document presents an overview of healthcare transformation through lean and six sigma methodologies, emphasizing the importance of continuous improvement and waste reduction for organizational success. It details case studies that illustrate how these principles have led to significant improvements in primary care settings and orthopedics, highlighting methodologies like value stream analysis and simulation for optimizing patient flow and operational efficiency. Key tools and outcomes from these approaches demonstrate the potential for enhanced patient care and reduced costs in the healthcare industry.