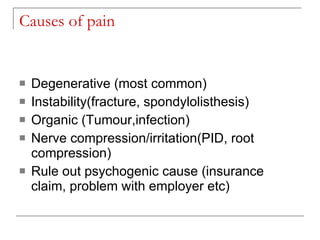
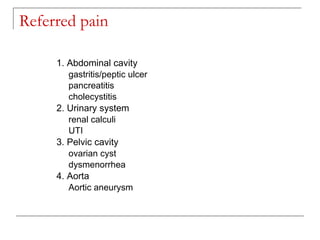
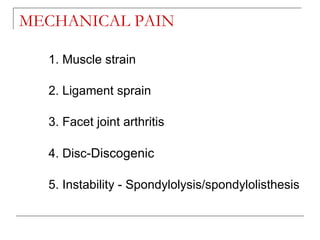
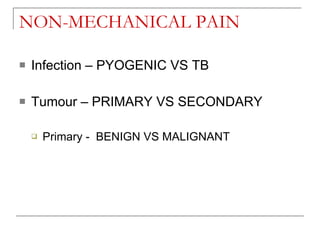
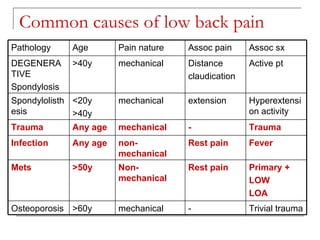
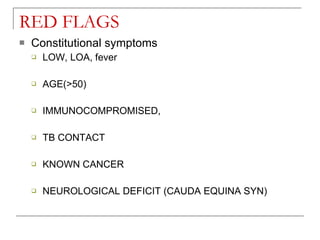
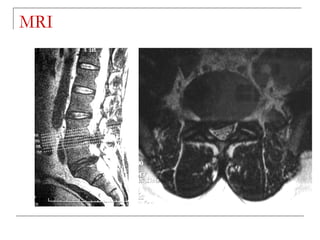
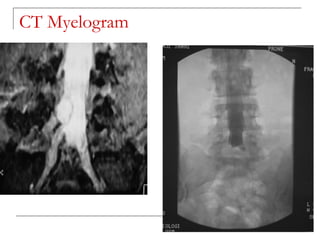
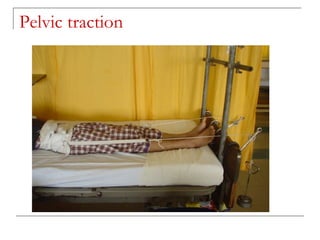
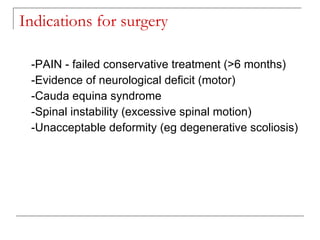
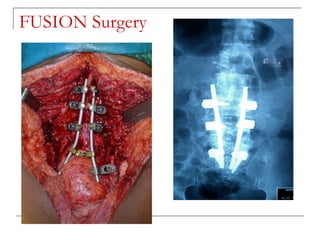
This document discusses low back pain, which is very common among working adults. It presents in people over 45 years old and is usually caused by degenerative changes or instability in the lumbosacral region of the spine. While 80% of cases resolve with conservative treatment like rest, heat, and over-the-counter medications, 5-10% may require surgery for issues like nerve compression, instability, or deformity. The document outlines approaches to evaluating and diagnosing the cause of low back pain through history, physical exam, imaging studies, and outlines treatment approaches including conservative care, injections, and surgical options.