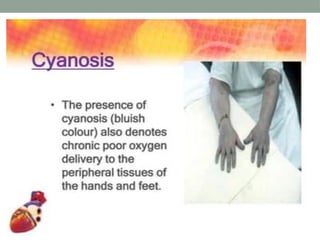
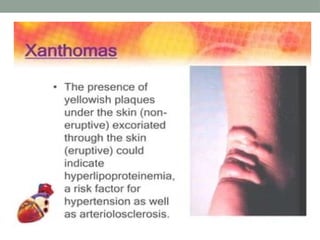
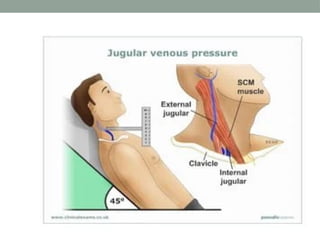
The document outlines a comprehensive cardiovascular assessment process, including physical assessments such as inspection, palpation, and auscultation of various heart and vascular structures. It details specific signs and tests, such as capillary refill time and jugular venous pressure, as well as laboratory tests and diagnostic procedures like EKG, chest X-ray, and echocardiography. The document emphasizes the importance of these evaluations in assessing cardiac function and detecting abnormalities.