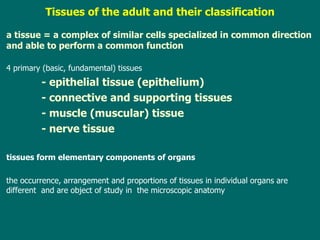
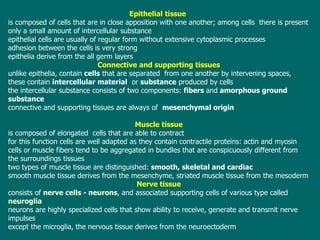
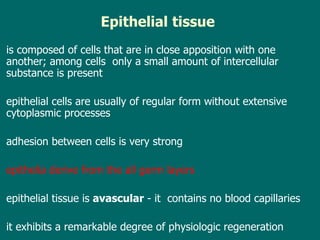
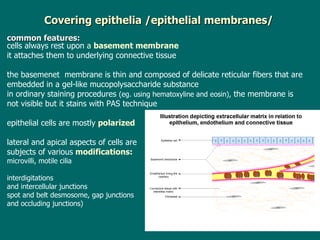
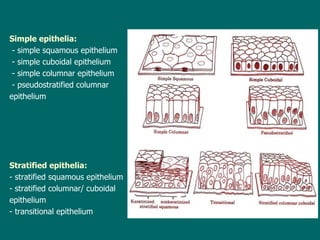
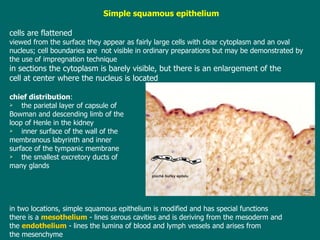
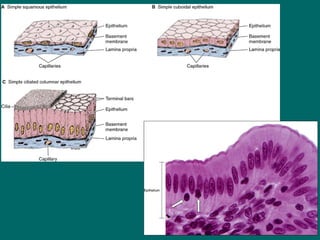
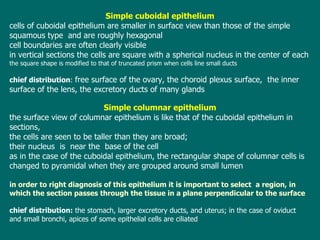
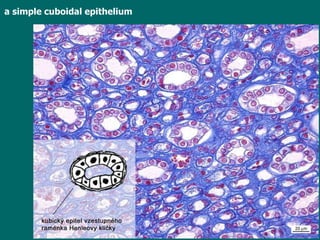
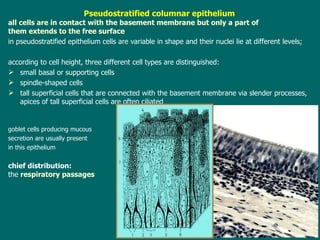
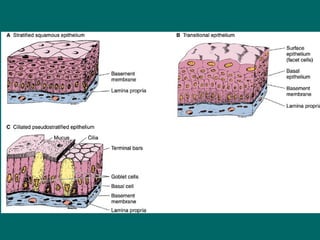
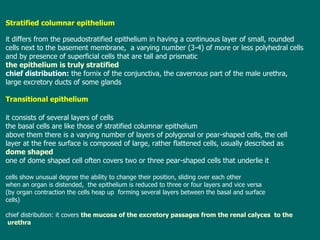
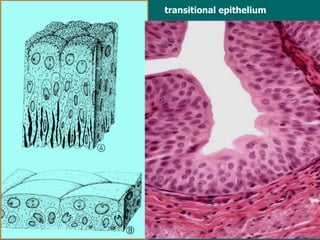
This document provides an overview of epithelial tissue, including its definition, classification, characteristics, and locations in the body. It discusses the four primary tissue types - epithelial, connective, muscle, and nerve tissue. It focuses on epithelial tissue, describing the two main types (simple and stratified), their subtypes based on cell shape, and examples of each epithelium's location and function. Key points covered include that epithelial tissue lines surfaces, derives from all germ layers, and lacks blood vessels.