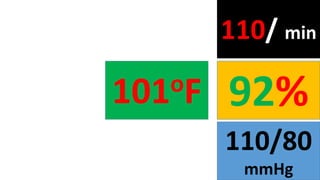
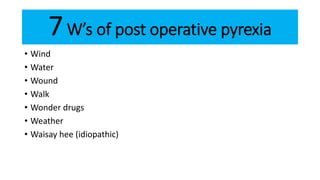
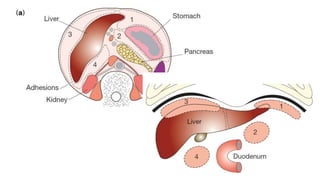
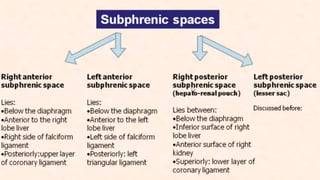
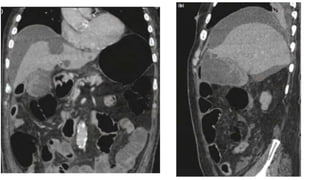
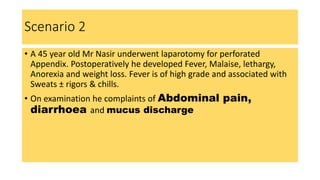
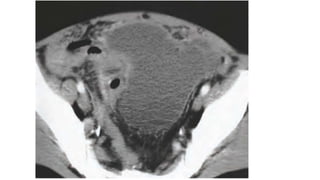
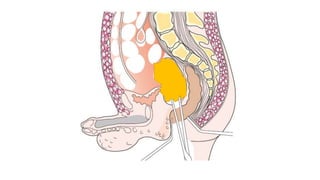
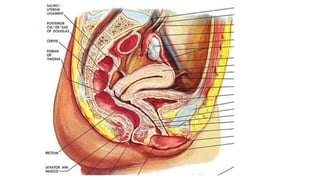
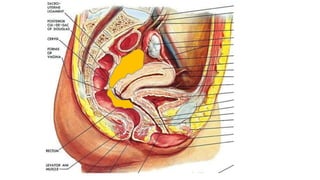
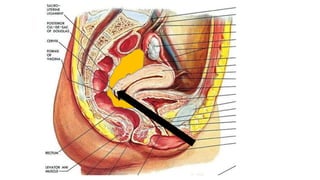
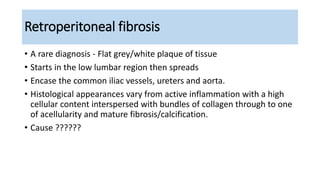
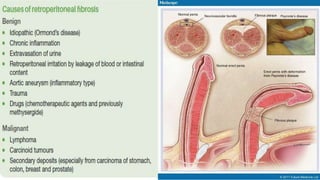
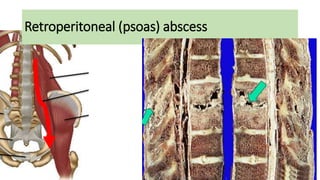
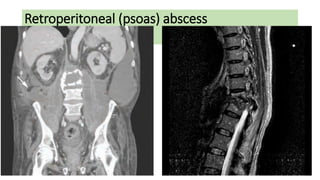
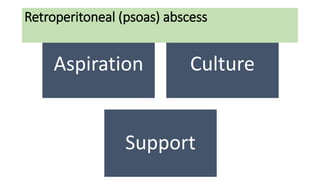
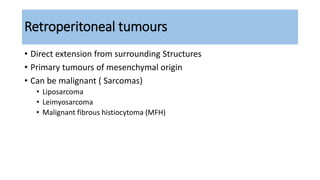
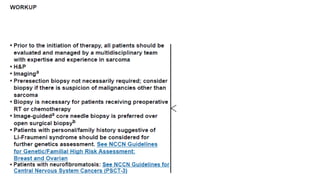
The document discusses various causes of intra-abdominal and retroperitoneal abscesses following surgery. It describes a case of a patient who underwent laparotomy for perforated duodenal perforation and subsequently developed fever and other symptoms. Possible causes discussed include plug leakage, abscess formation, or other sources of postoperative pyrexia. It then provides details on retroperitoneal abscesses, fibrosis, and tumors - outlining characteristics, causes, clinical features, and treatment considerations for each.