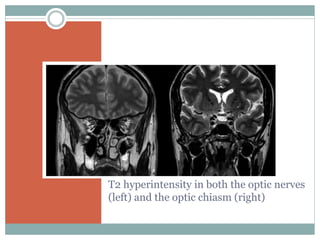
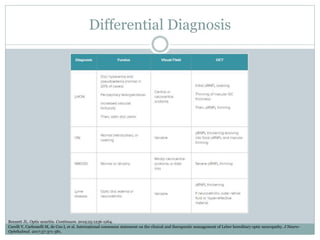
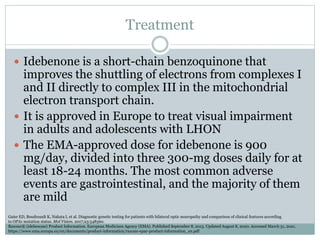
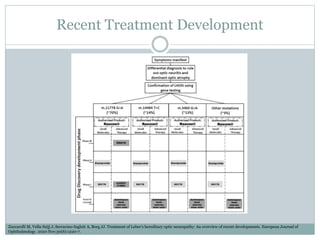
Leber's hereditary optic neuropathy (LHON) is a maternally inherited mitochondrial disease characterized by acute or subacute, bilateral, painless loss of central vision. It is caused by specific mitochondrial DNA mutations and usually affects young adult males. Clinically, it presents with severe, permanent vision loss in one eye followed by the other within a year. Diagnosis is based on clinical features and identification of one of the three common mitochondrial DNA mutations. While there is no cure, idebenone is approved to treat visual impairment in LHON. Recent research focuses on developing new treatments targeting the underlying mitochondrial dysfunction.