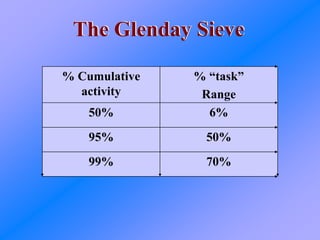
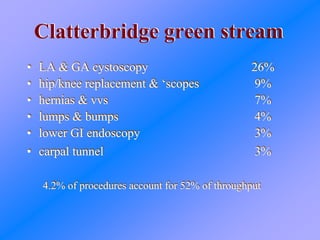
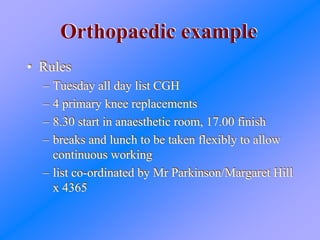
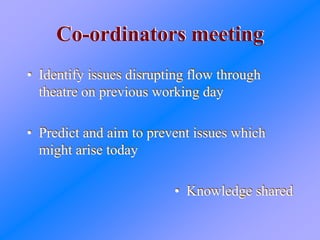
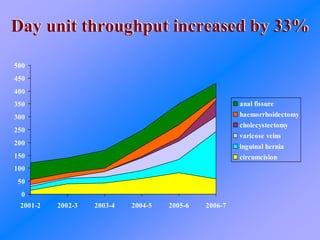
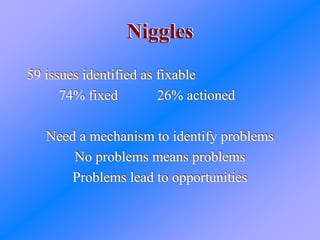
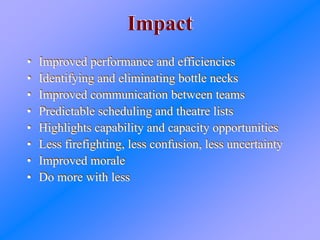
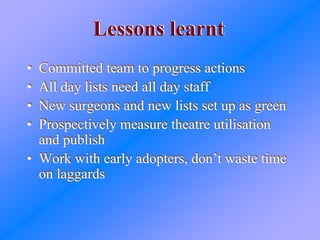
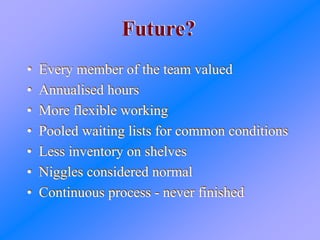
The document discusses using lean principles and value stream mapping to improve operating theatre utilization and patient flow at a hospital. It describes identifying high-volume procedures, standardizing equipment and scheduling for these "green stream" cases, and coordinating staff to allow continuous workflow. As a result, day unit throughput increased 33%, inpatient beds were reduced, and staff communicated better with fewer delays. Lessons included needing committed teams and measuring utilization continuously.