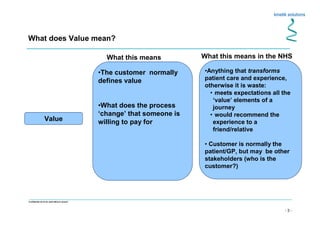
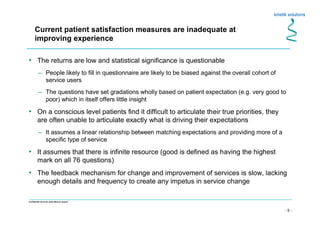
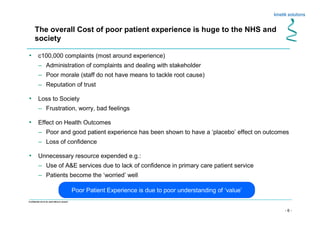
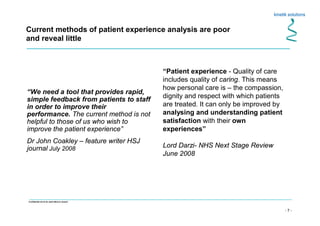
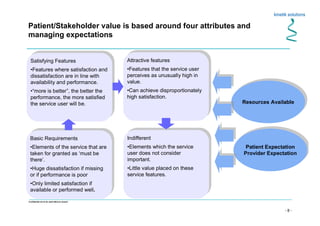
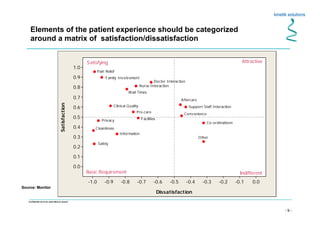
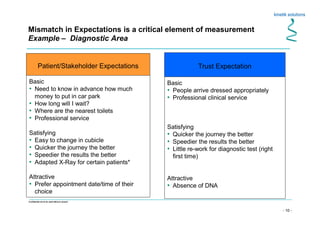
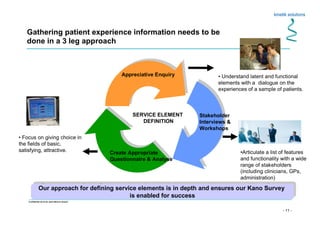
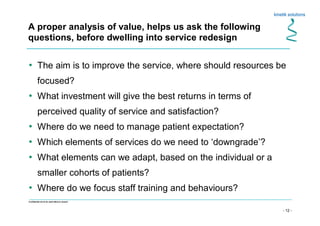
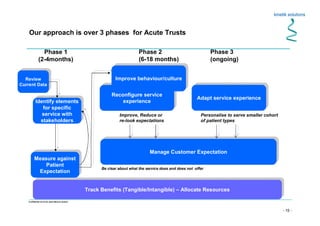
The document discusses lean principles and processes, with a focus on understanding value from the customer's perspective. It emphasizes removing waste, taking a bottom-up approach to identify value and waste, and allowing processes to flow with little command and control. The document also examines how to properly define and measure patient value in healthcare to improve patient experience and outcomes. It argues that current patient satisfaction measures are inadequate and that value should be explored from multiple stakeholder perspectives to guide sustainable service improvements.