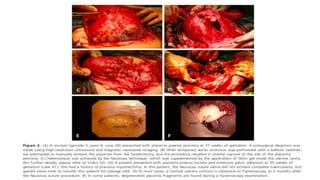
1) The Nausicaa compression suture is a novel technique for controlling major postpartum hemorrhage during cesarean sections.
2) It was tested on 68 patients with major PPH refractory to other conservative treatments.
3) The technique involves suturing the uterus from the outside in a horizontal fashion around the bleeding site to compress it.
4) It achieved hemostasis in 97% of cases and avoided hysterectomy, with minimal complications.