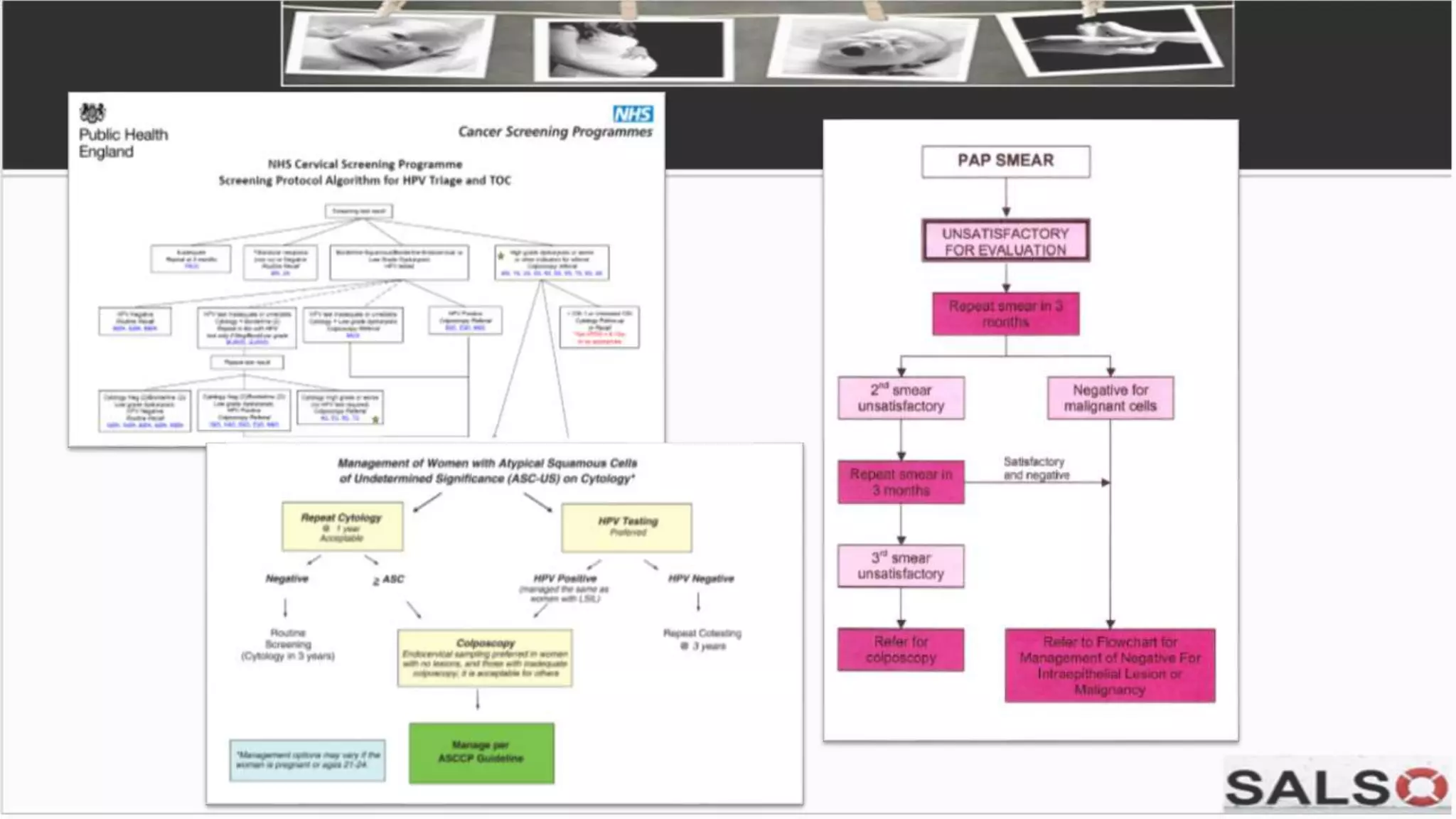
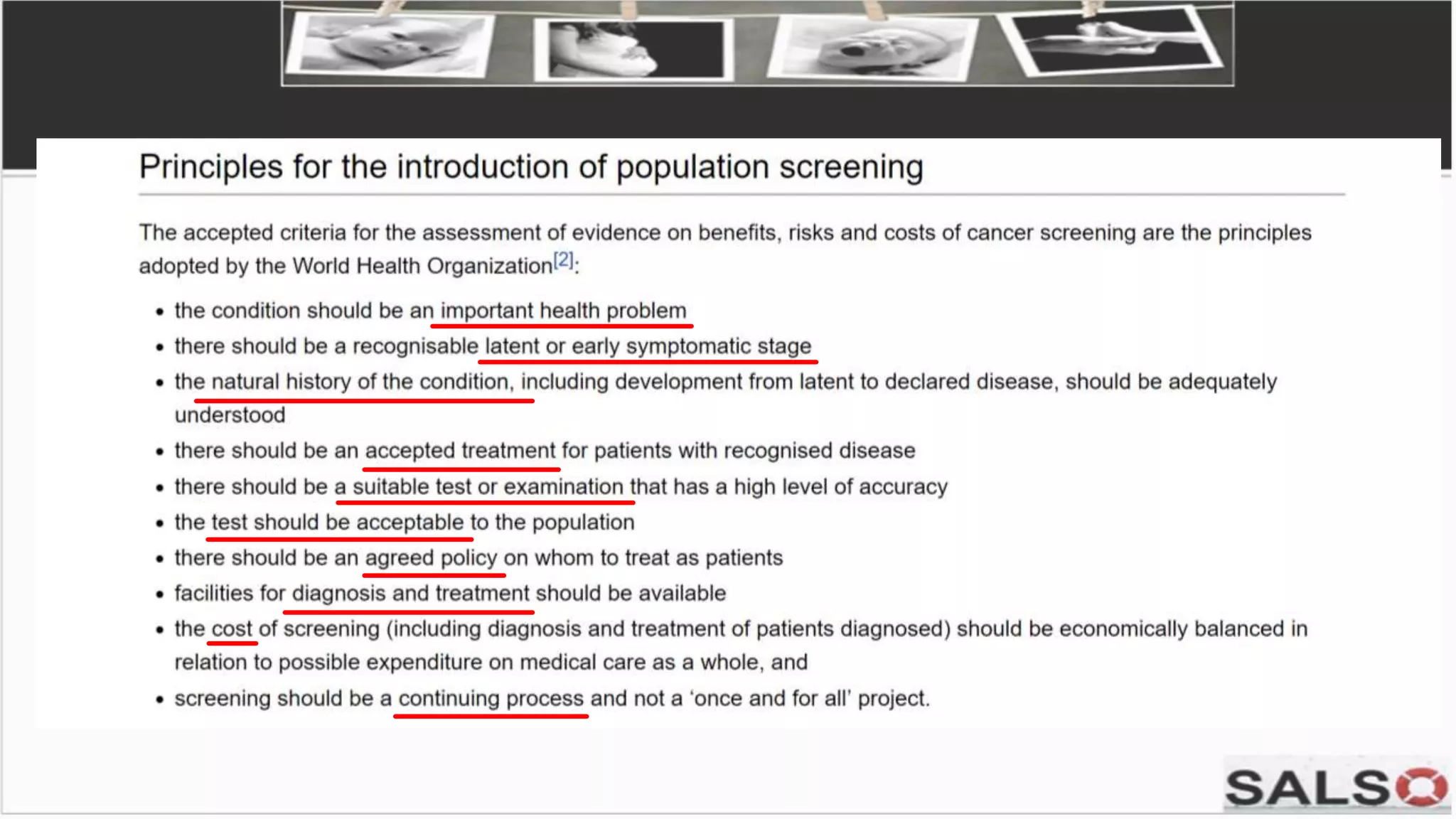
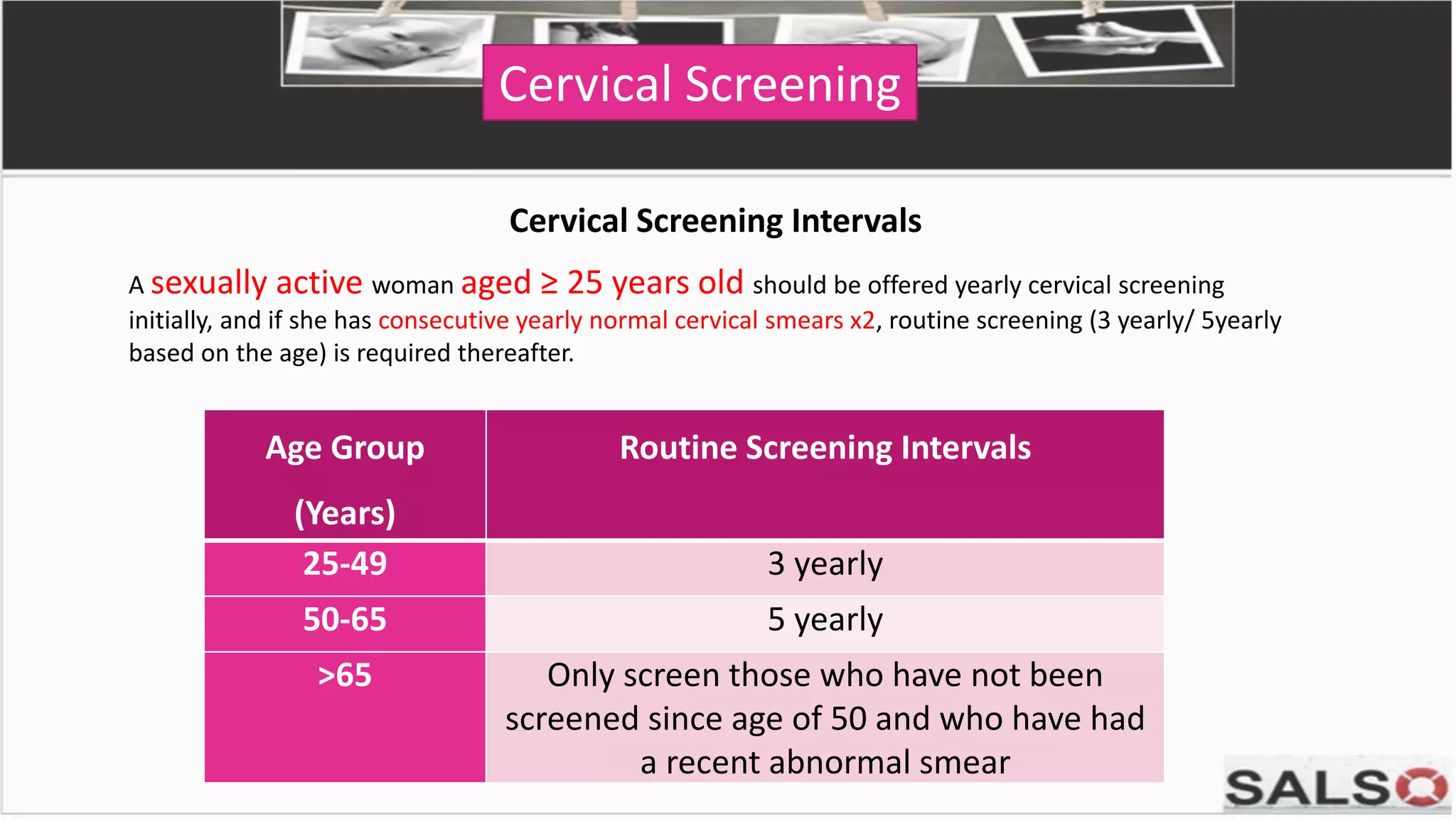
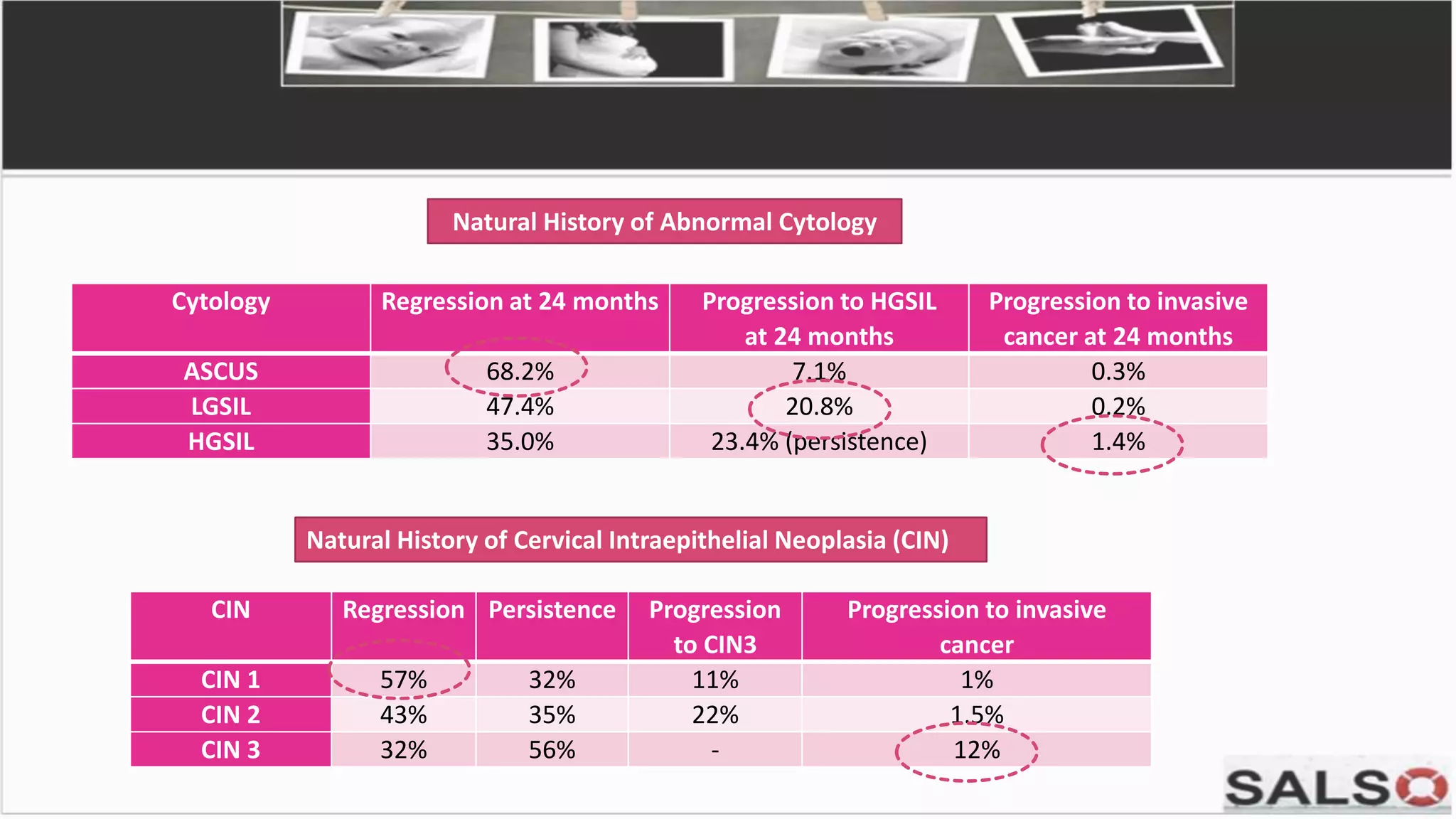
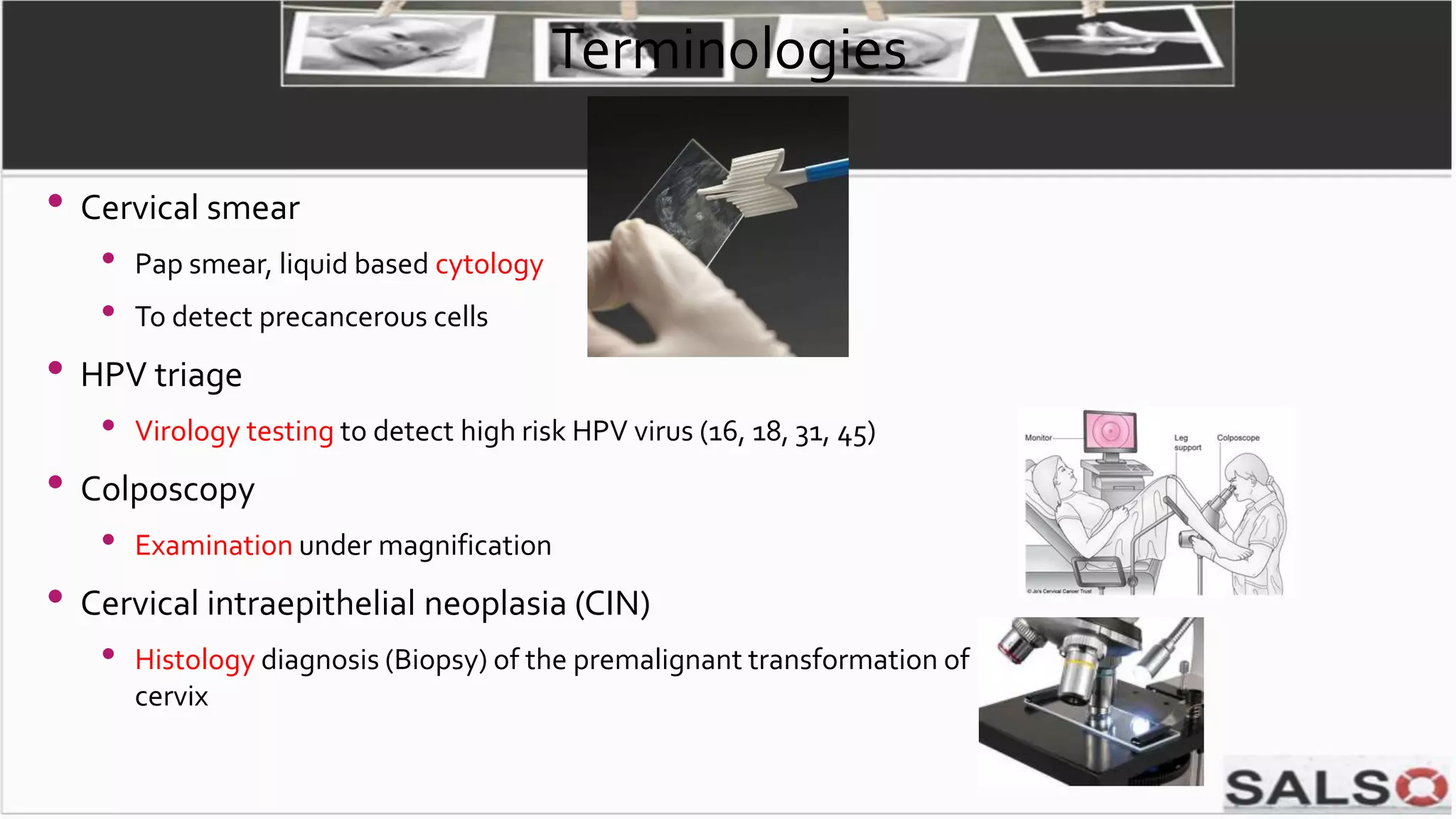
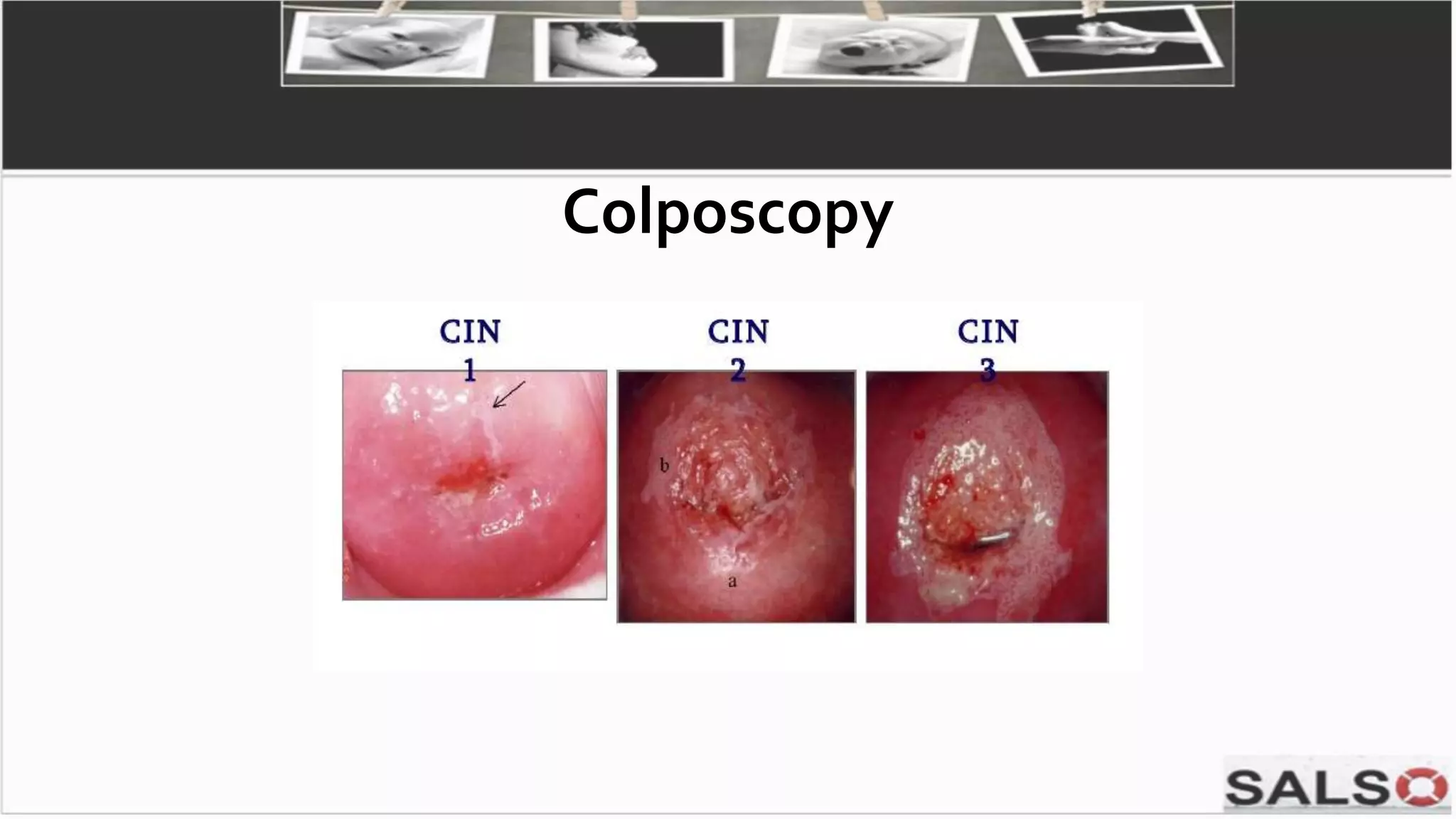
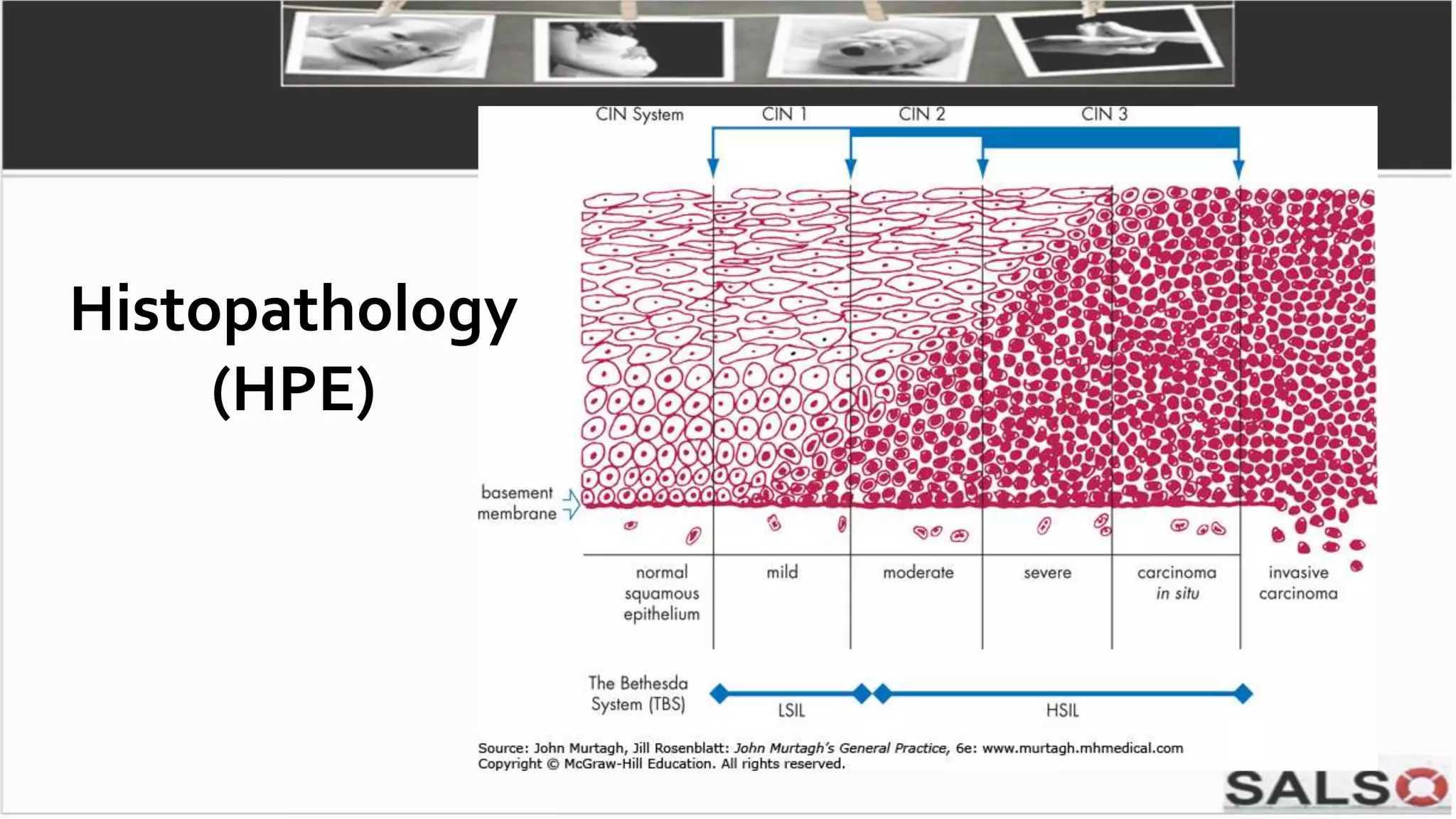
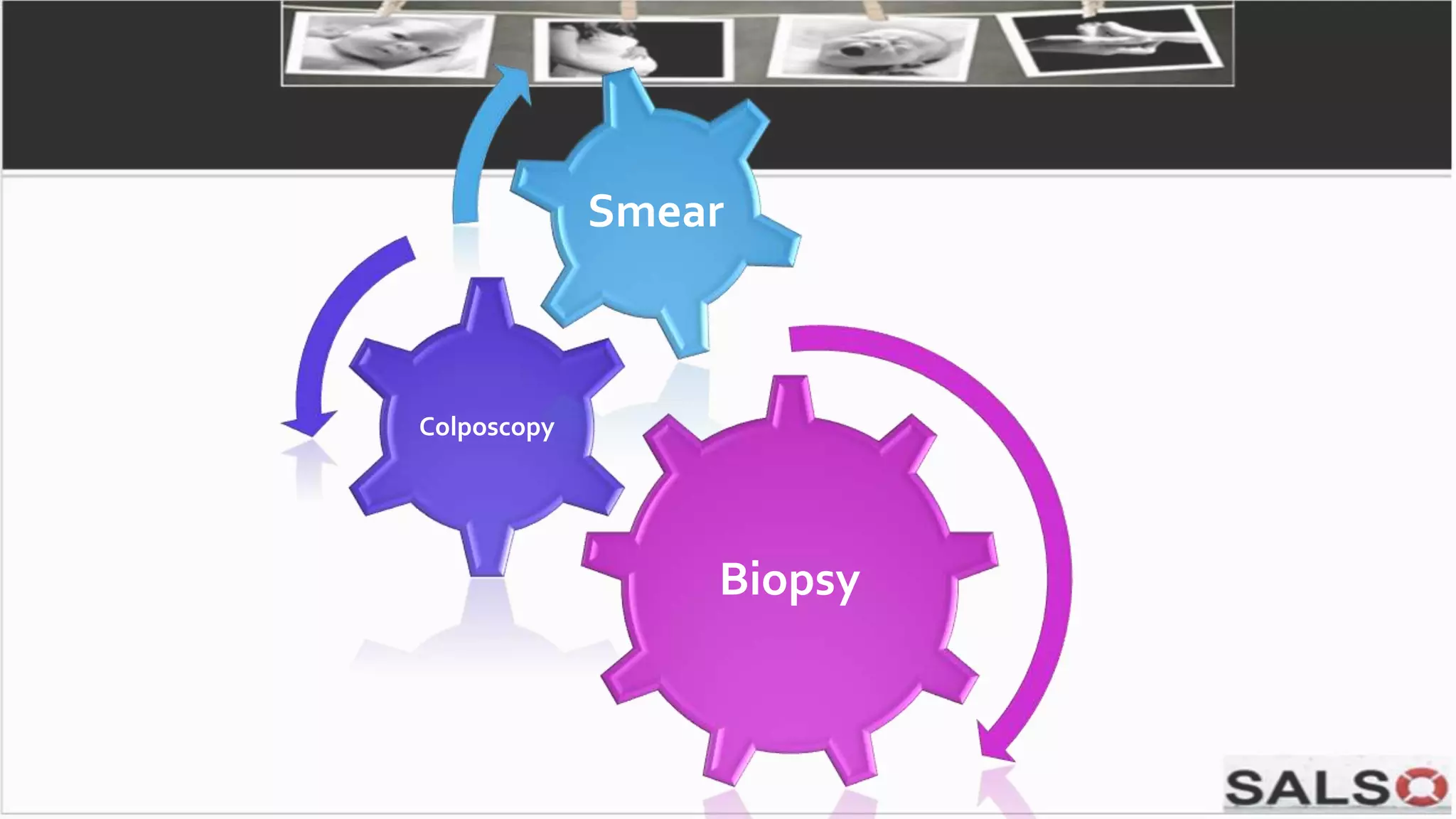
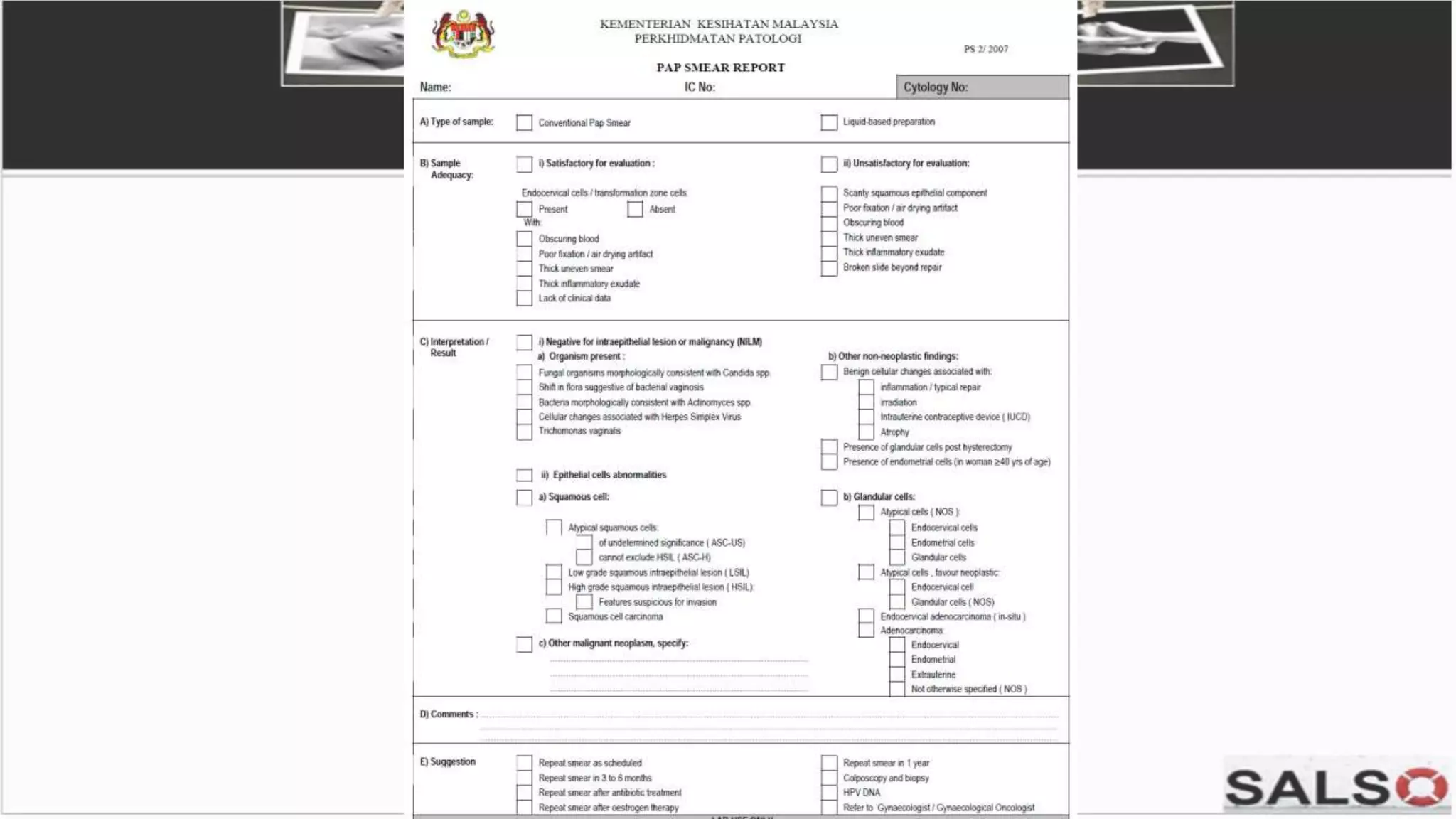
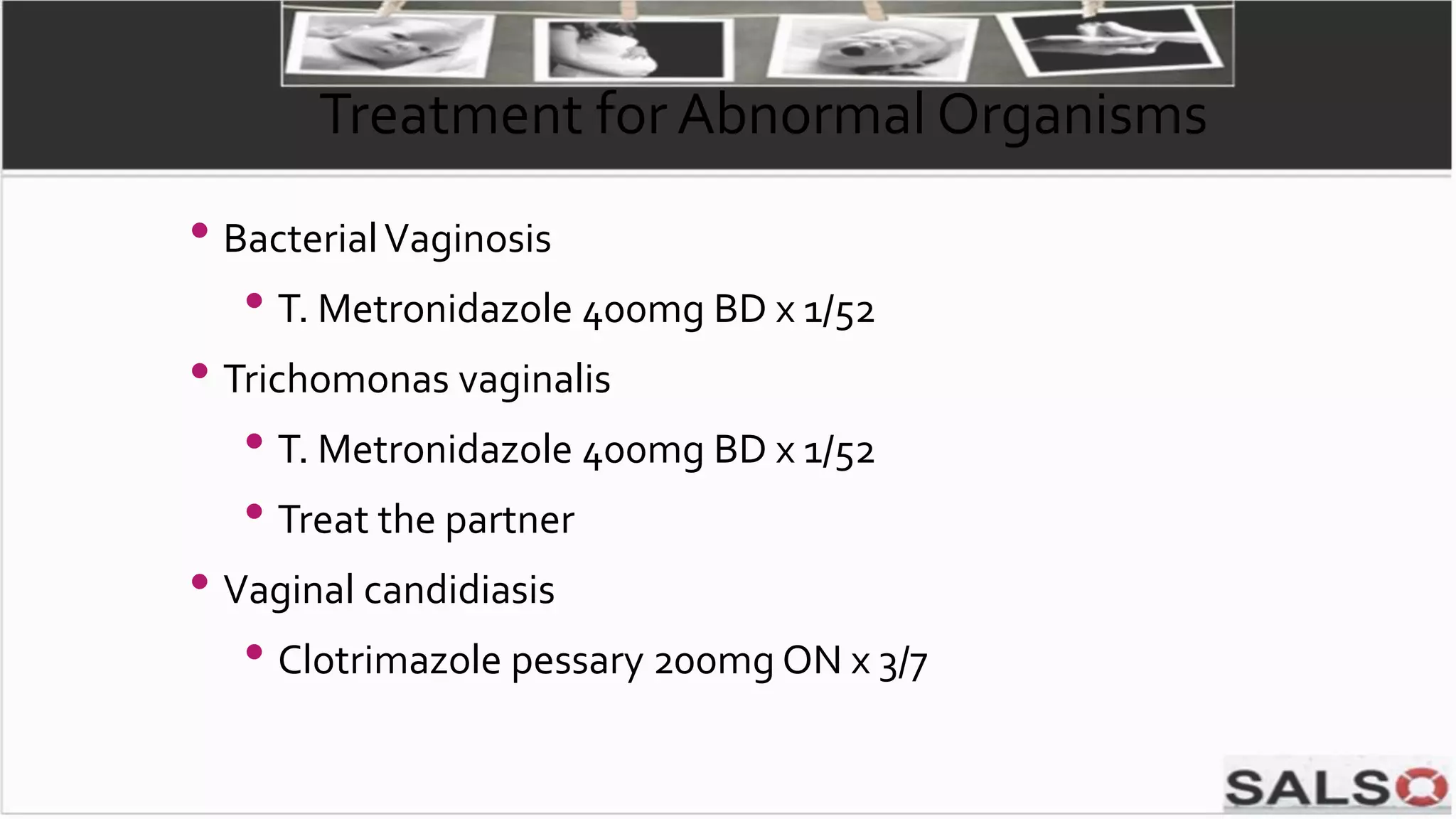
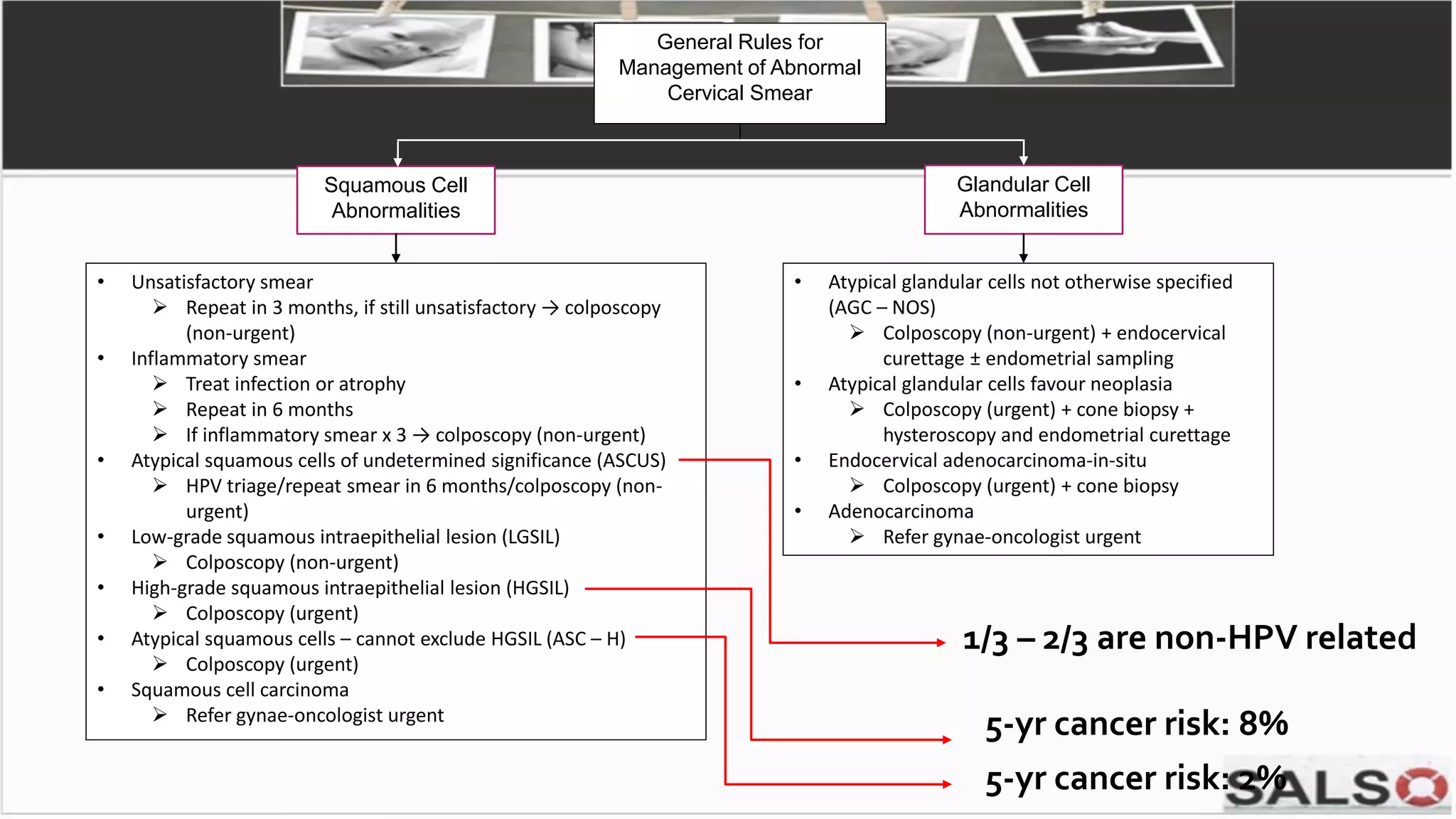
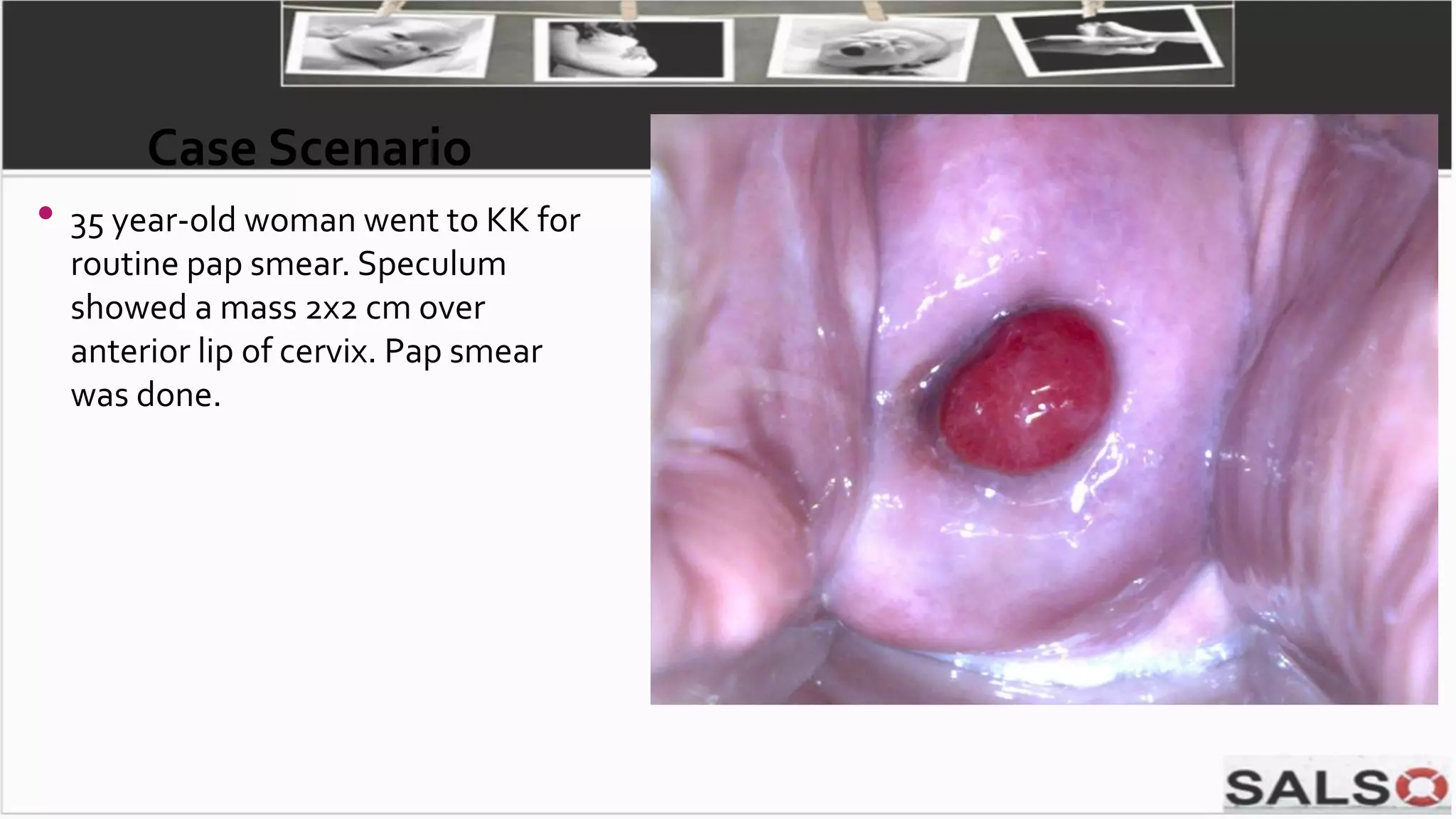
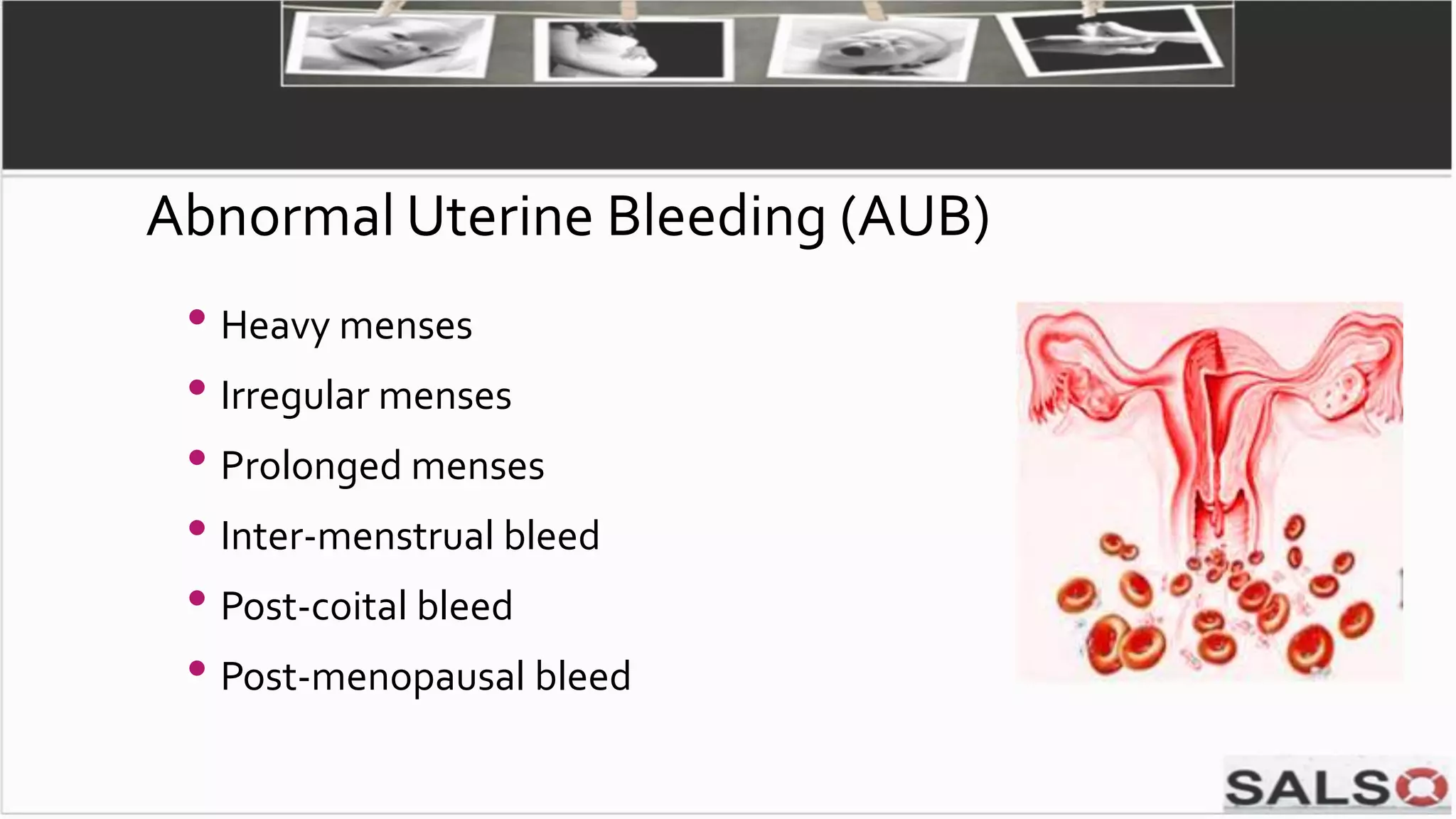
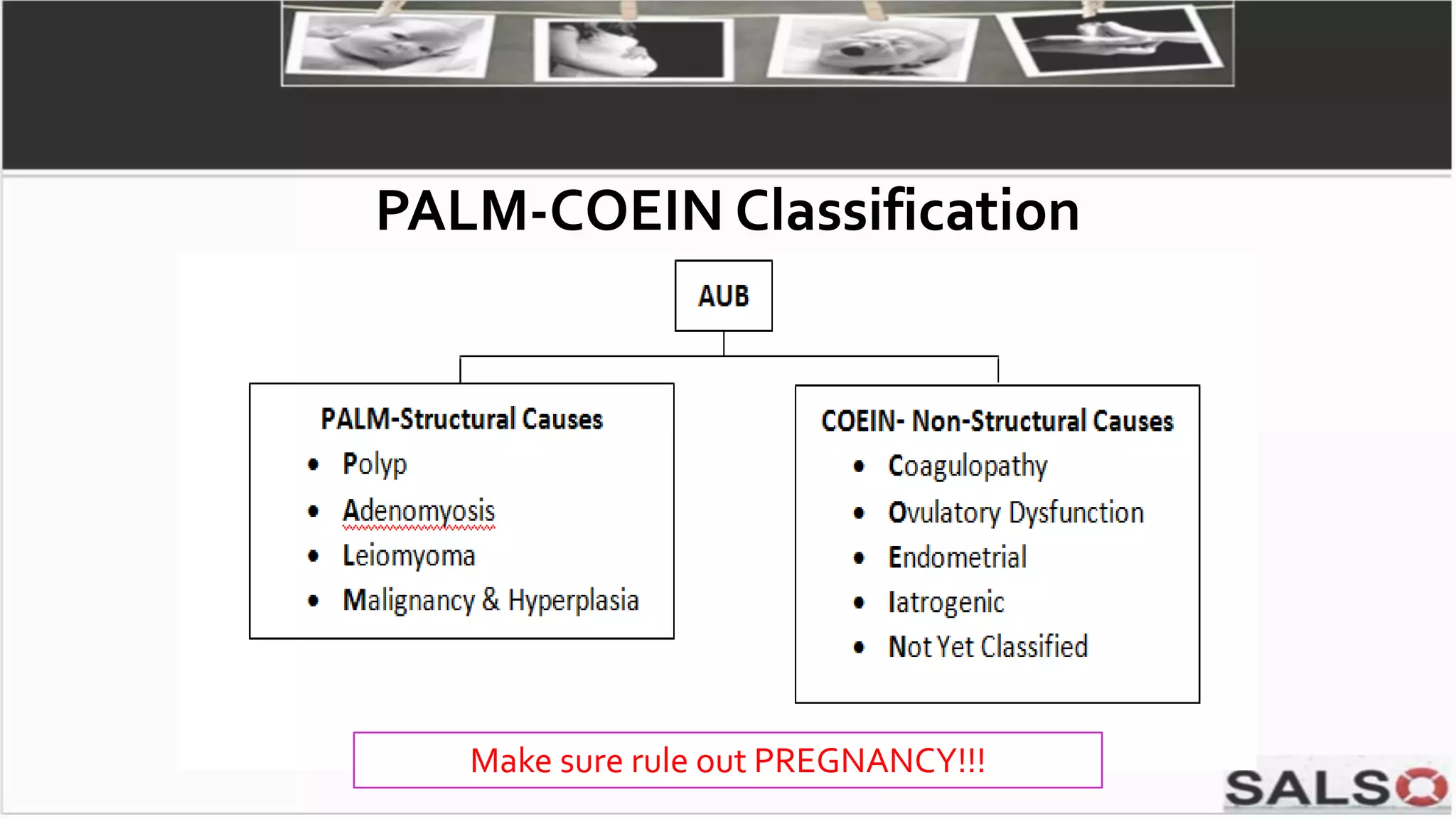
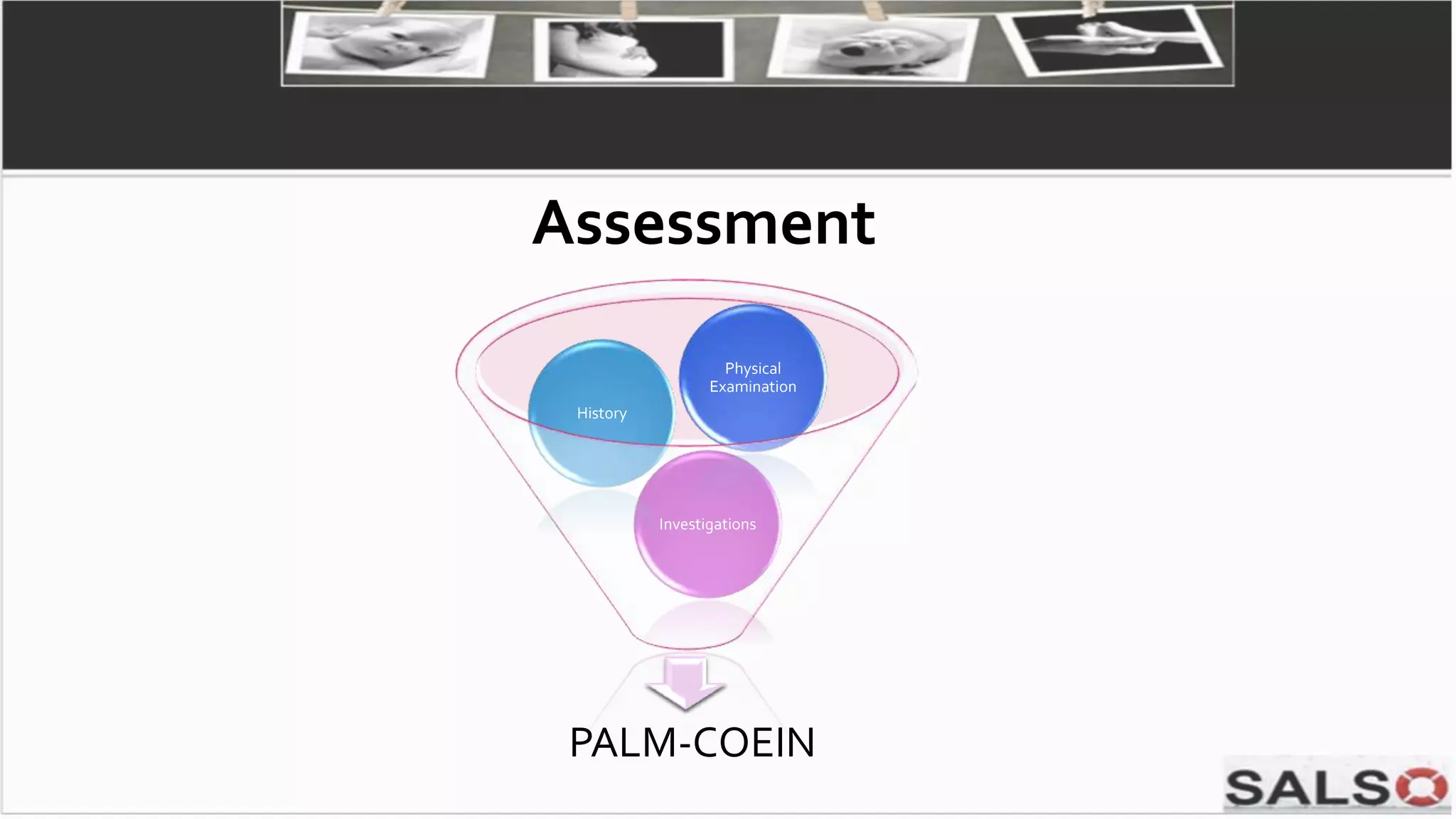
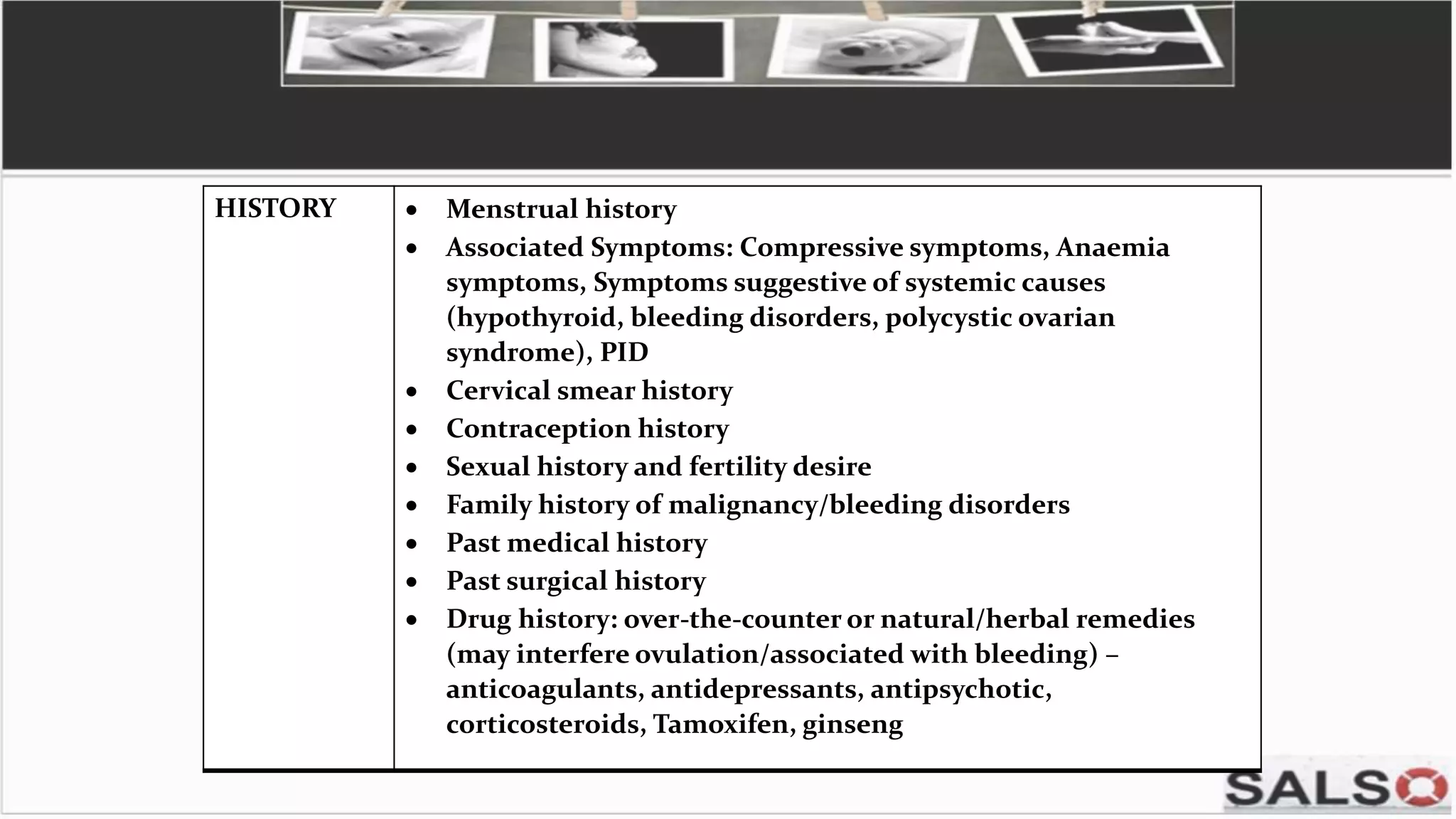
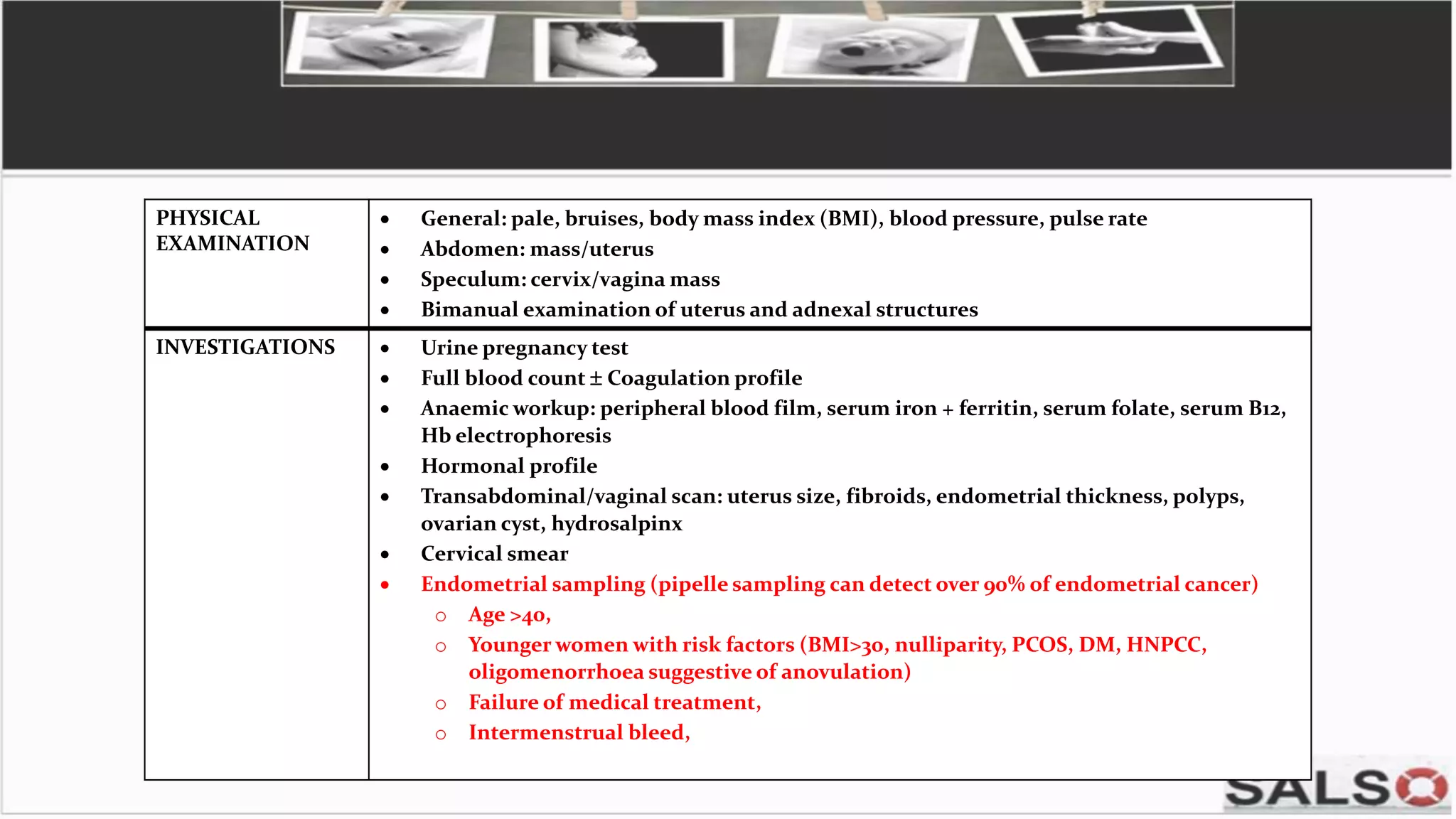
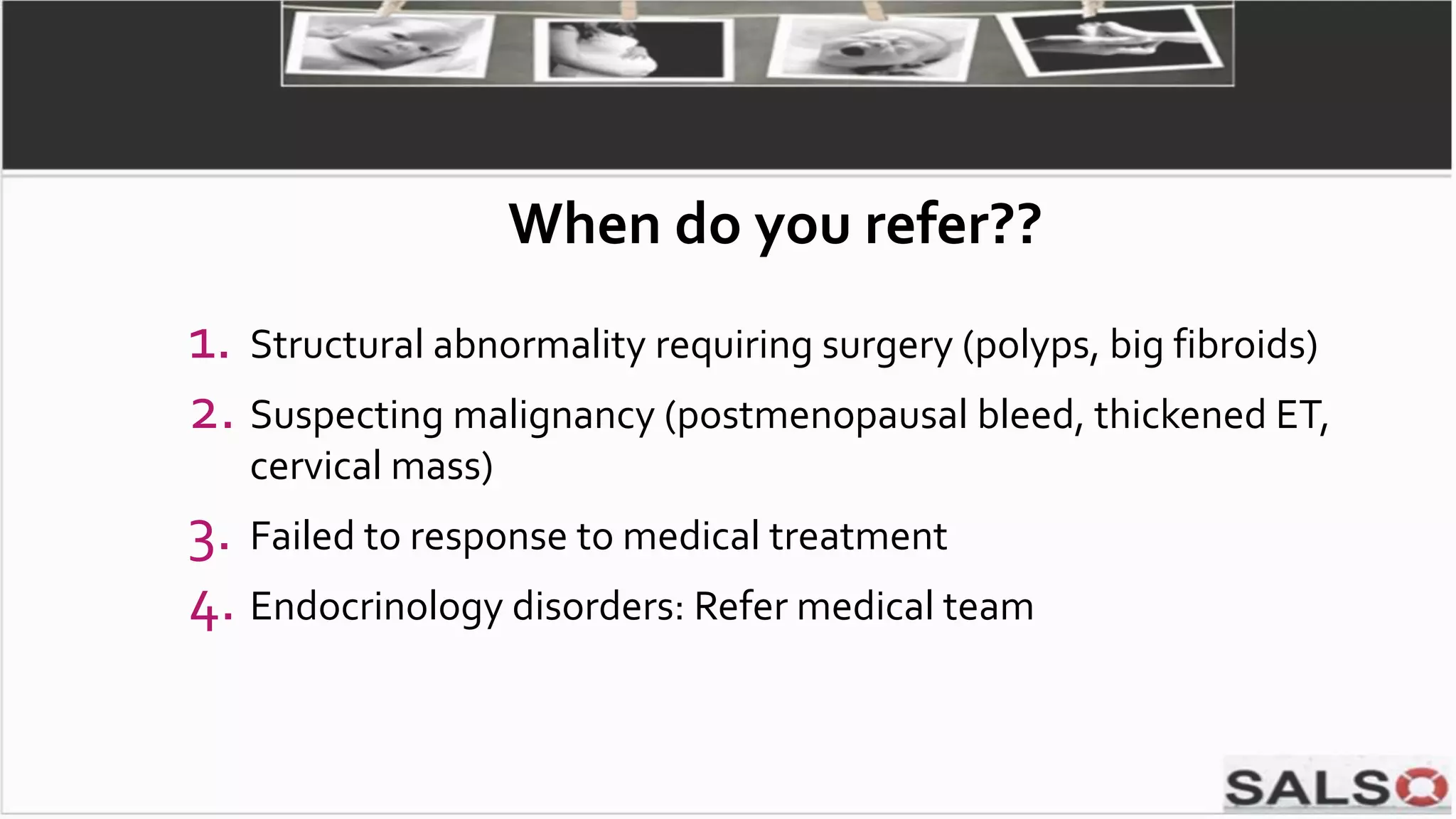
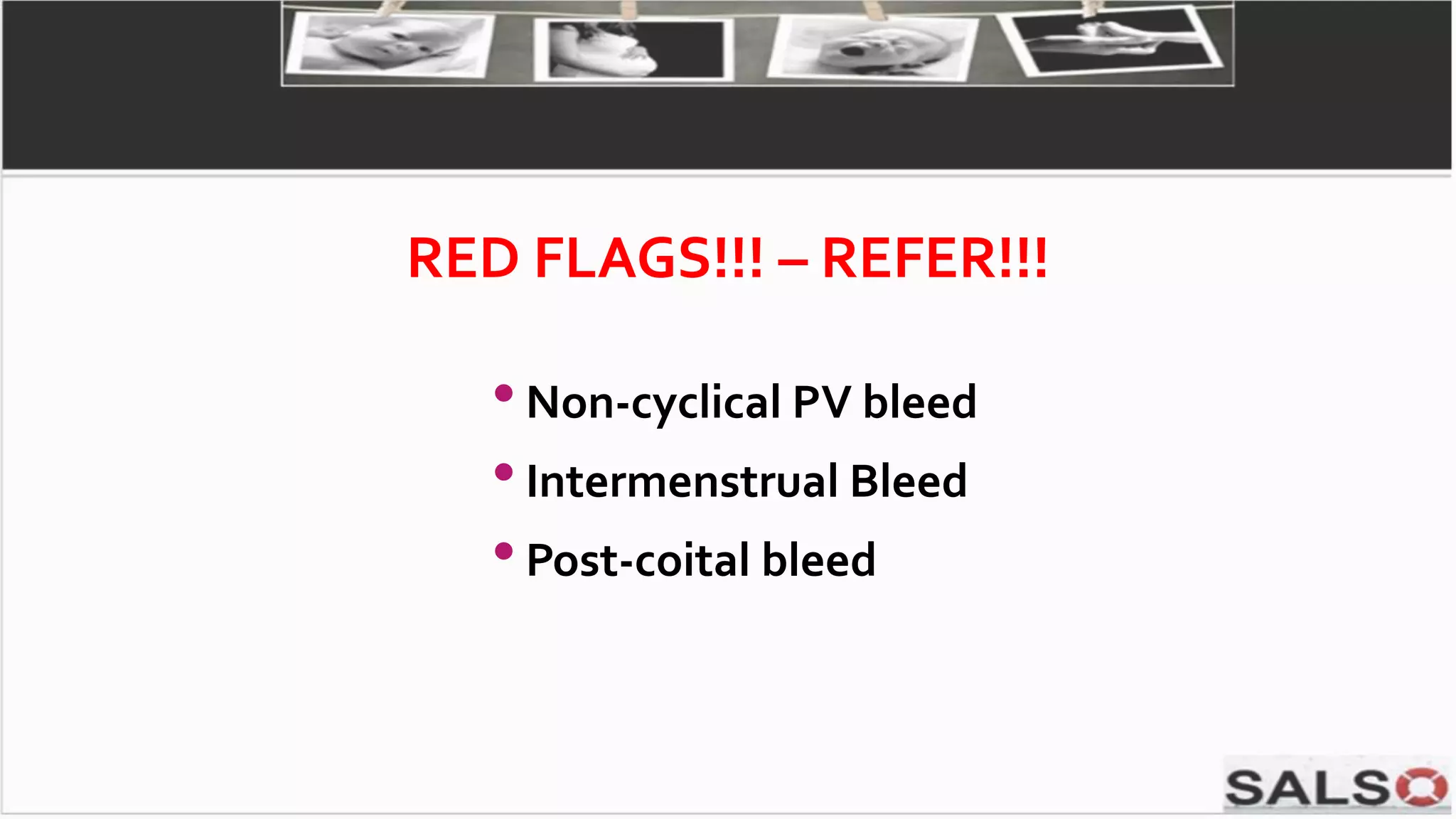
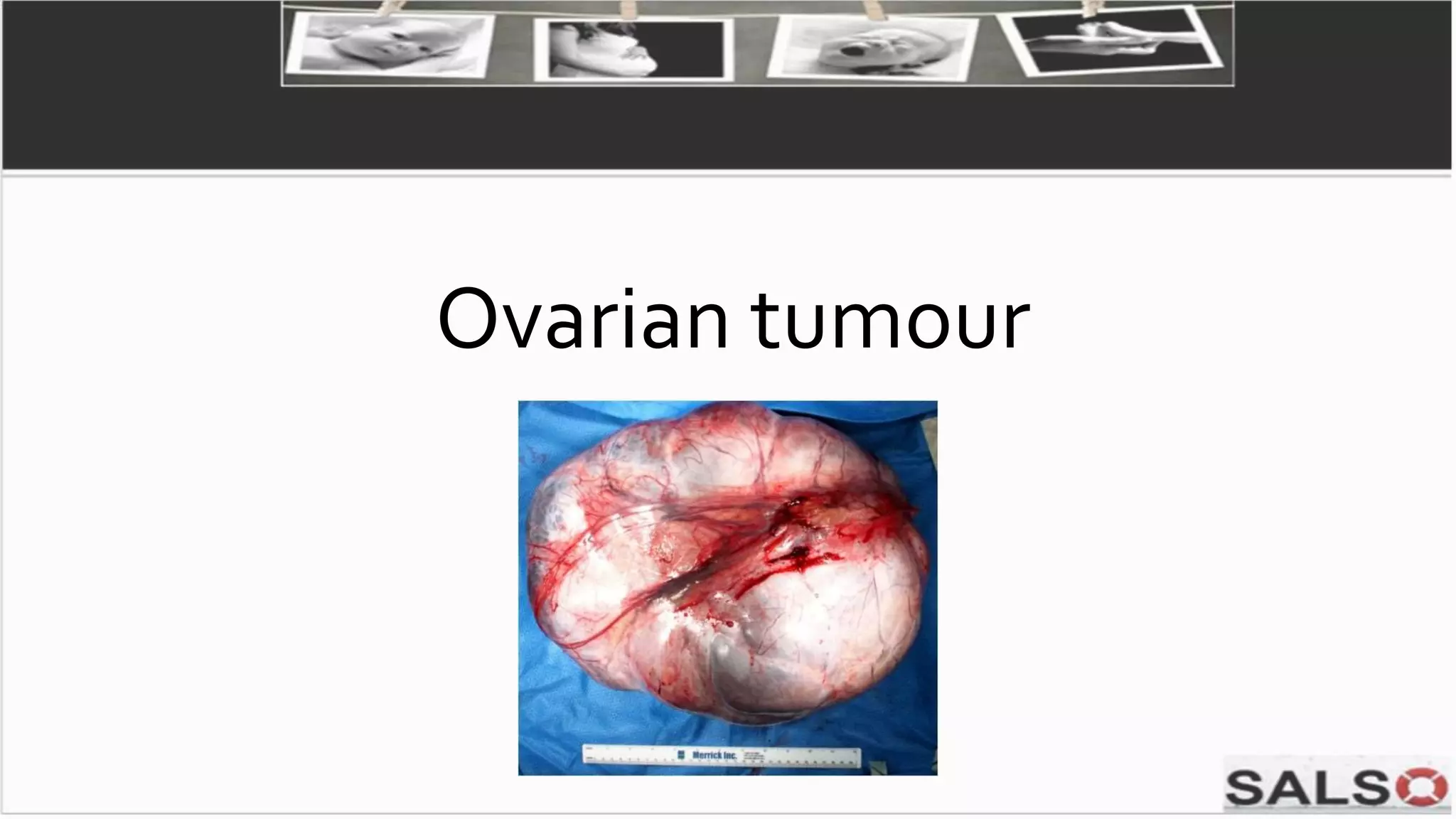
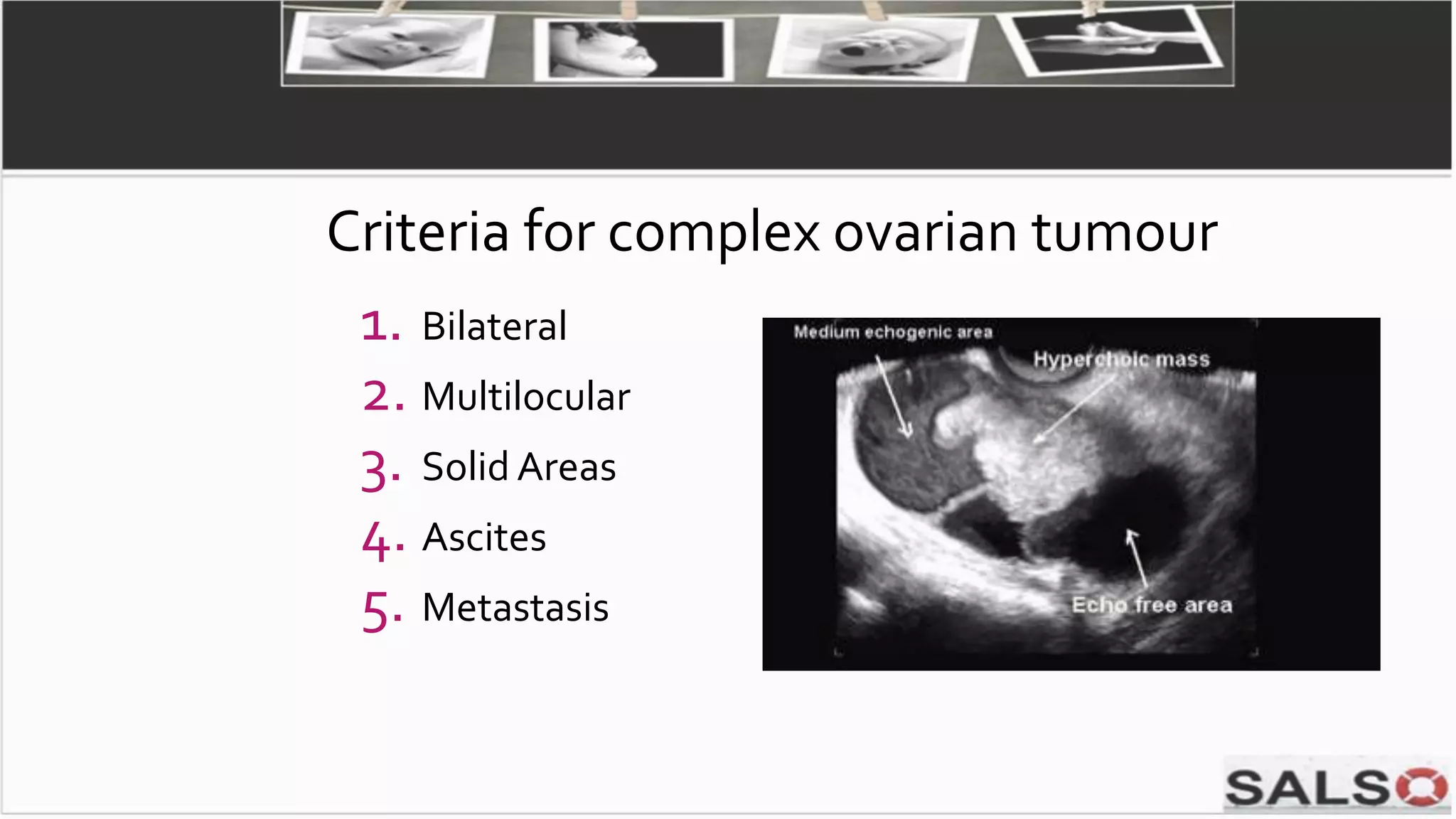
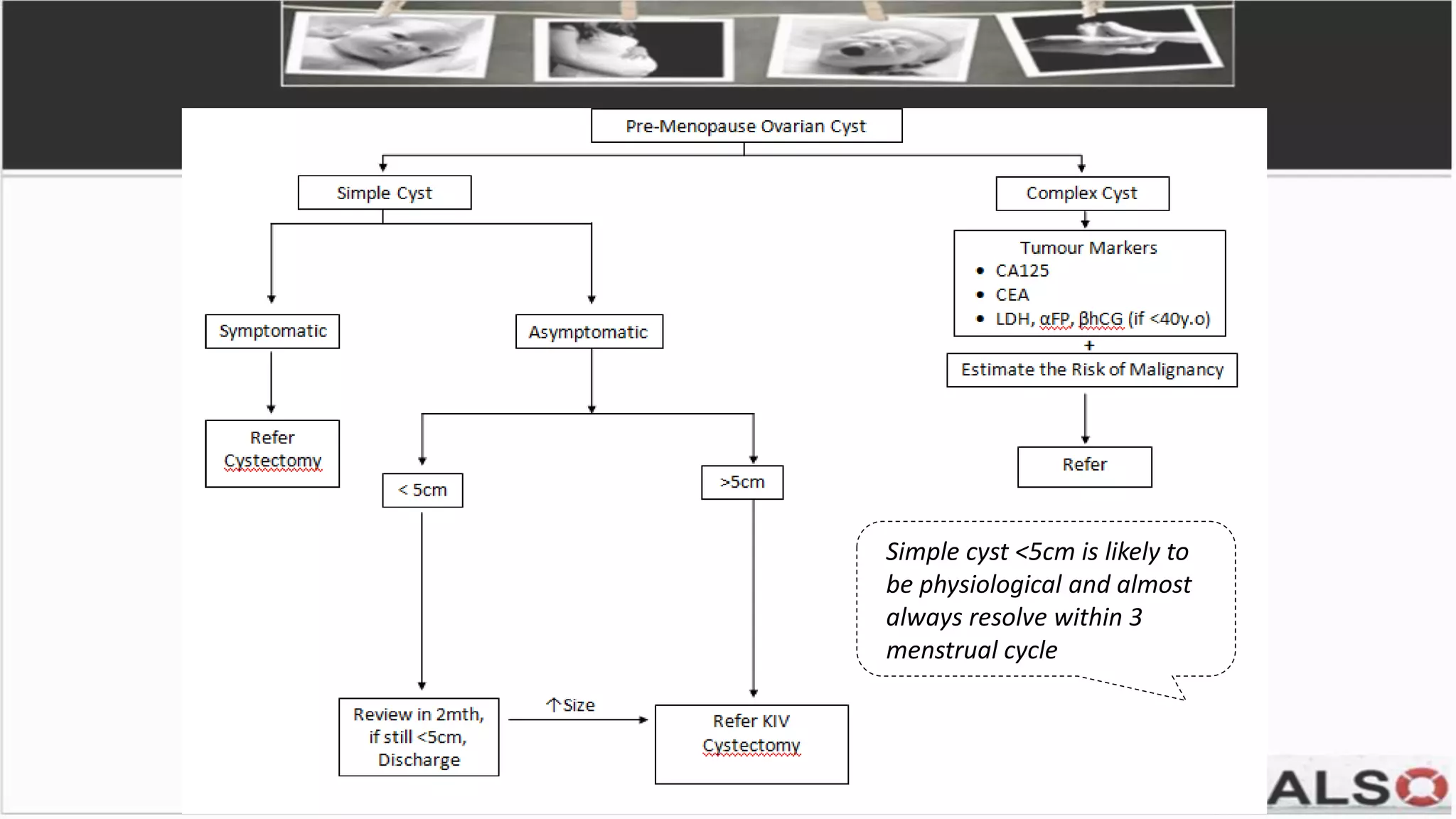
This document provides guidelines and pathways for gynaecology referrals in Sarawak, Malaysia. It includes standardized guidance for managing common conditions like cervical screening abnormalities, abnormal uterine bleeding, and ovarian tumors. The pathways are evidence-based and aim to enhance familiarization with management. They provide quick and easy referral processes for various gynaecological issues, including comprehensive summaries of evaluation, treatment recommendations, and referral criteria. The goal is to standardize care and ensure fast access to specialist evaluation when needed.