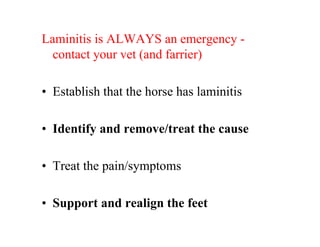
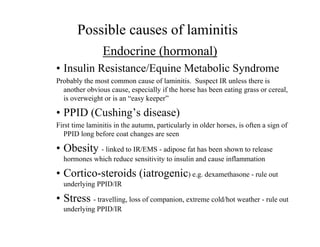
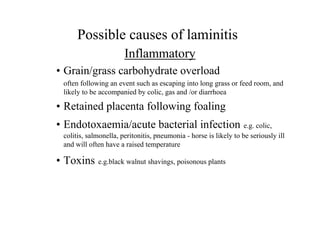
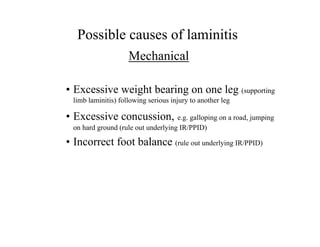
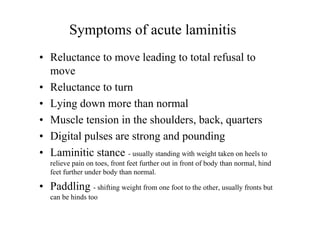
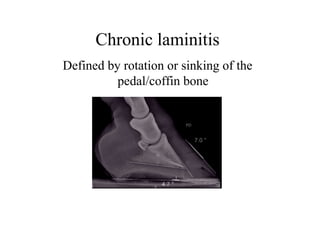
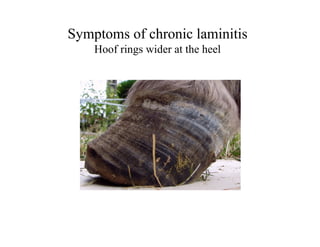
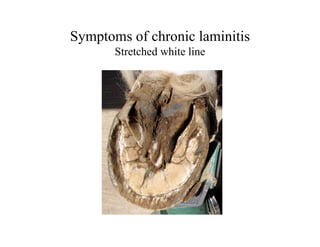
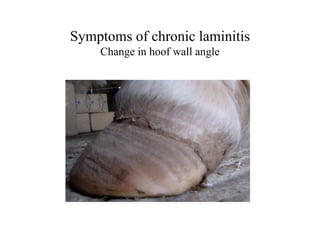
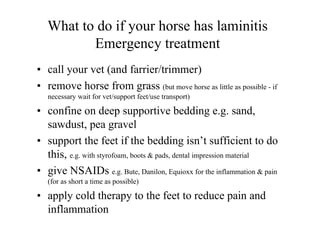
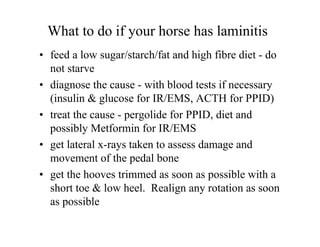
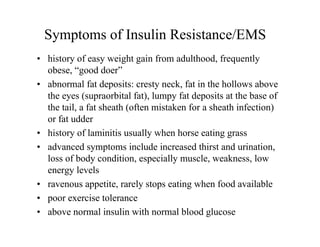
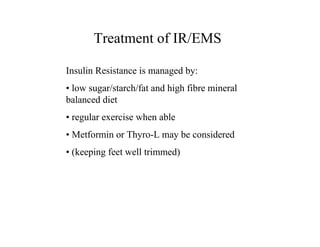
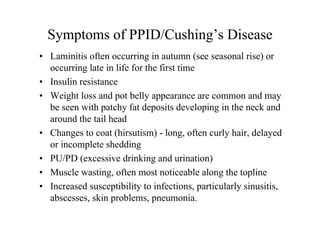
The document provides a comprehensive overview of laminitis in horses, highlighting its causes, symptoms, and treatments. It emphasizes the importance of recognizing the condition as an emergency, working with veterinarians, and implementing preventative measures to avoid laminitis recurrence. Key factors such as obesity, insulin resistance, and hormonal issues like PPID are detailed as significant contributors to the disease.