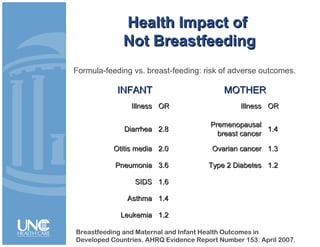
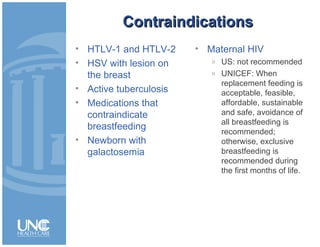
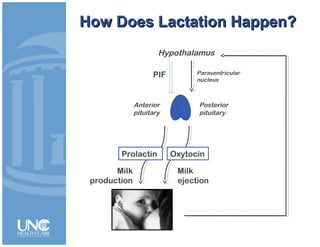
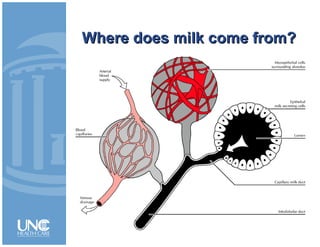
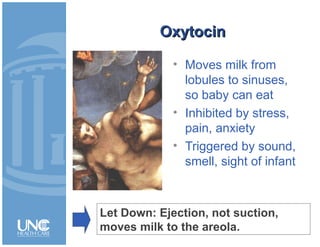
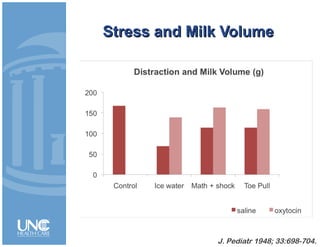
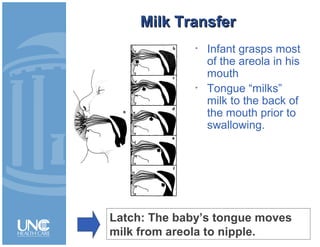
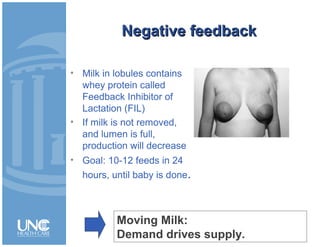
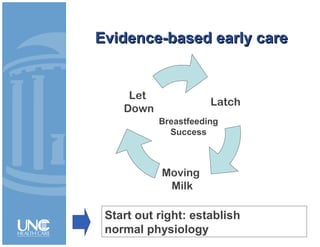
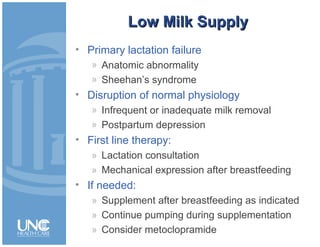
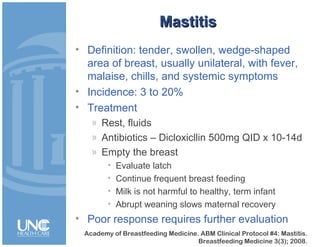
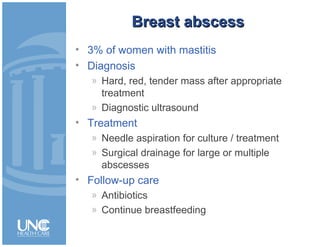
Breastfeeding provides significant health benefits to both infants and mothers by reducing the risk of various illnesses. The document discusses the physiology of lactation, including the roles of prolactin and oxytocin in milk production and ejection. It also covers common breastfeeding problems like low milk supply, mastitis, and breast abscess, providing diagnostic criteria and treatment recommendations. Maintaining proper latching, frequent feeding to stimulate supply, and emptying the breast are emphasized as ways to support breastfeeding success and maternal recovery from issues.