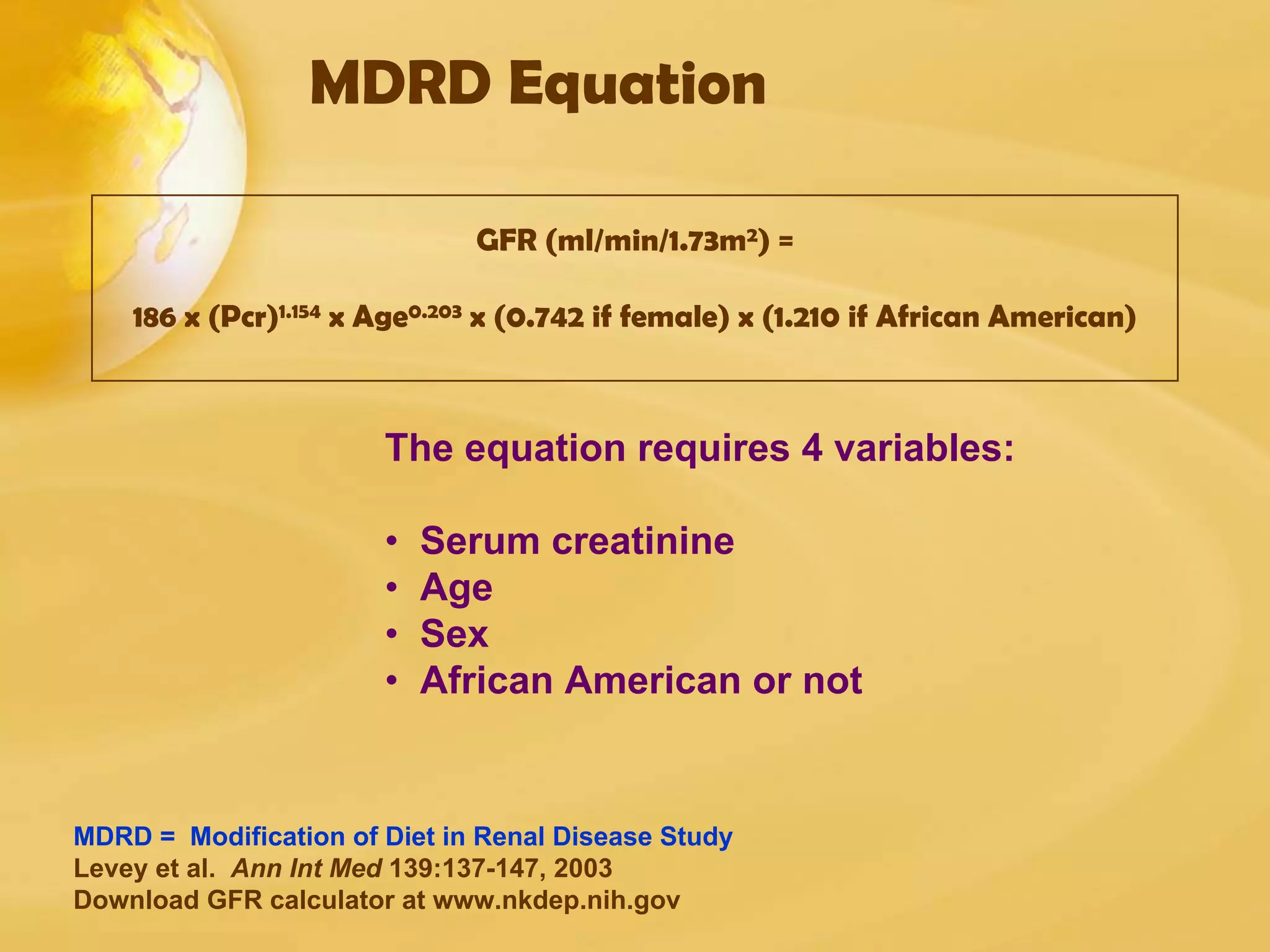
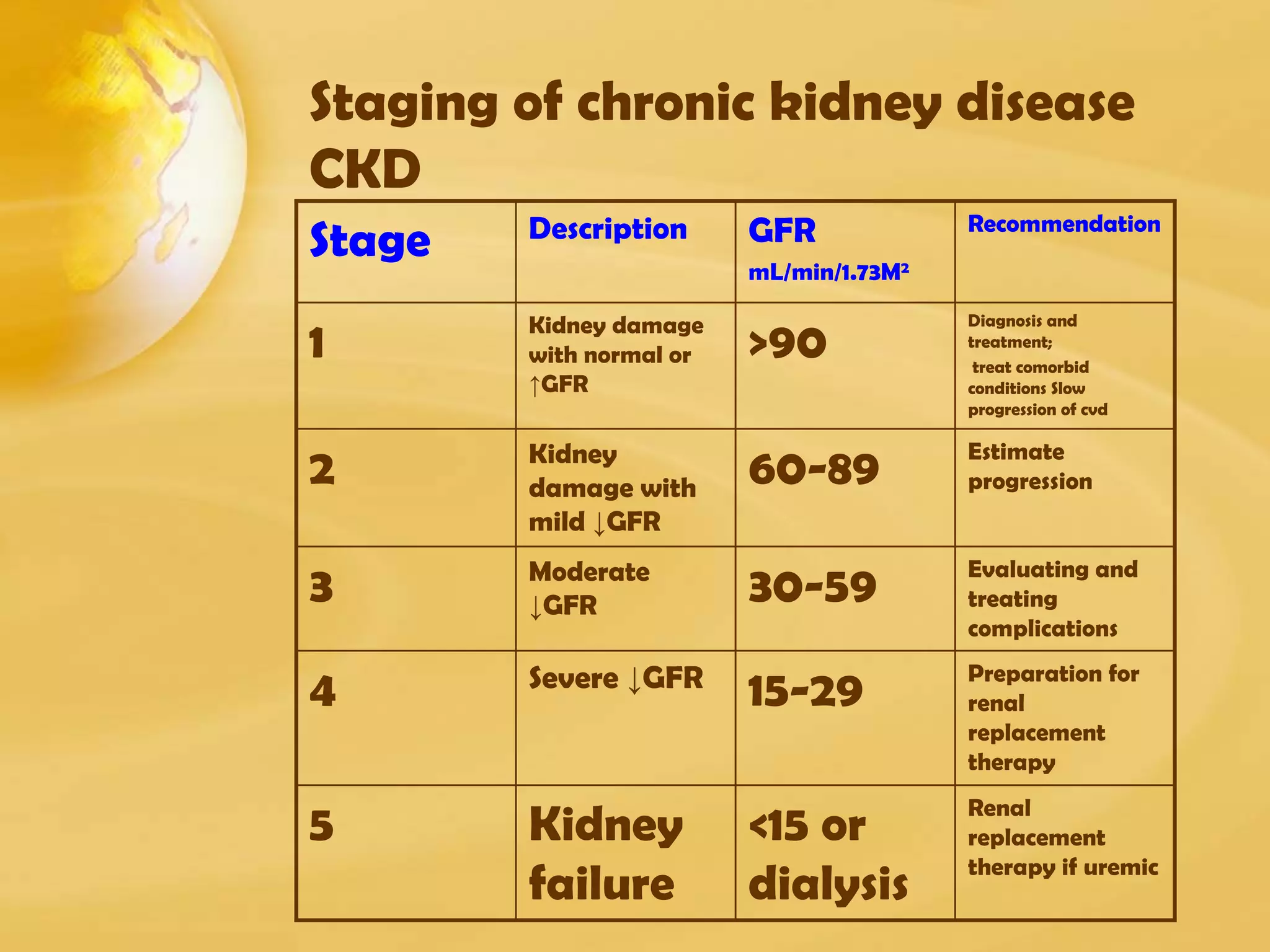
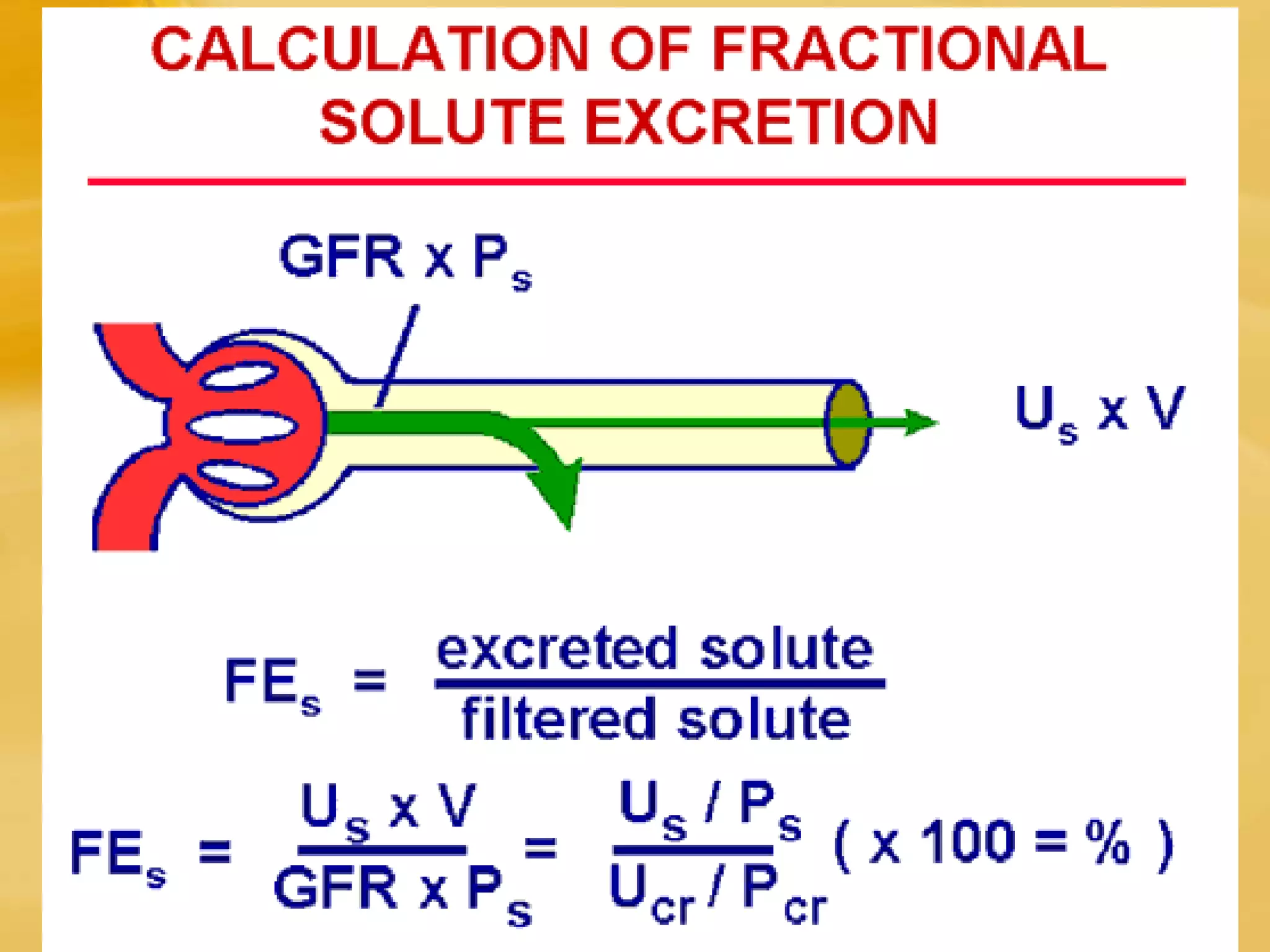
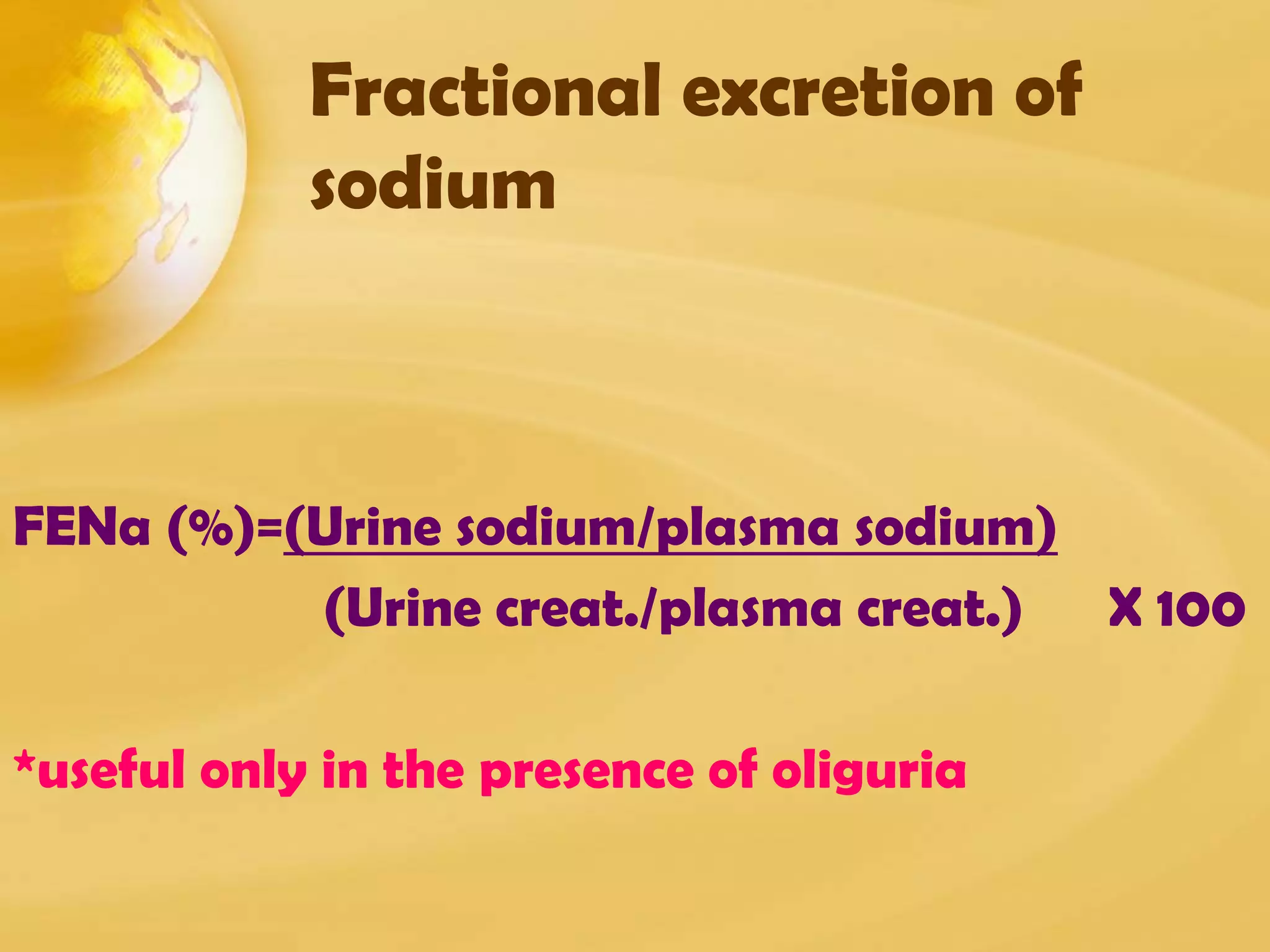
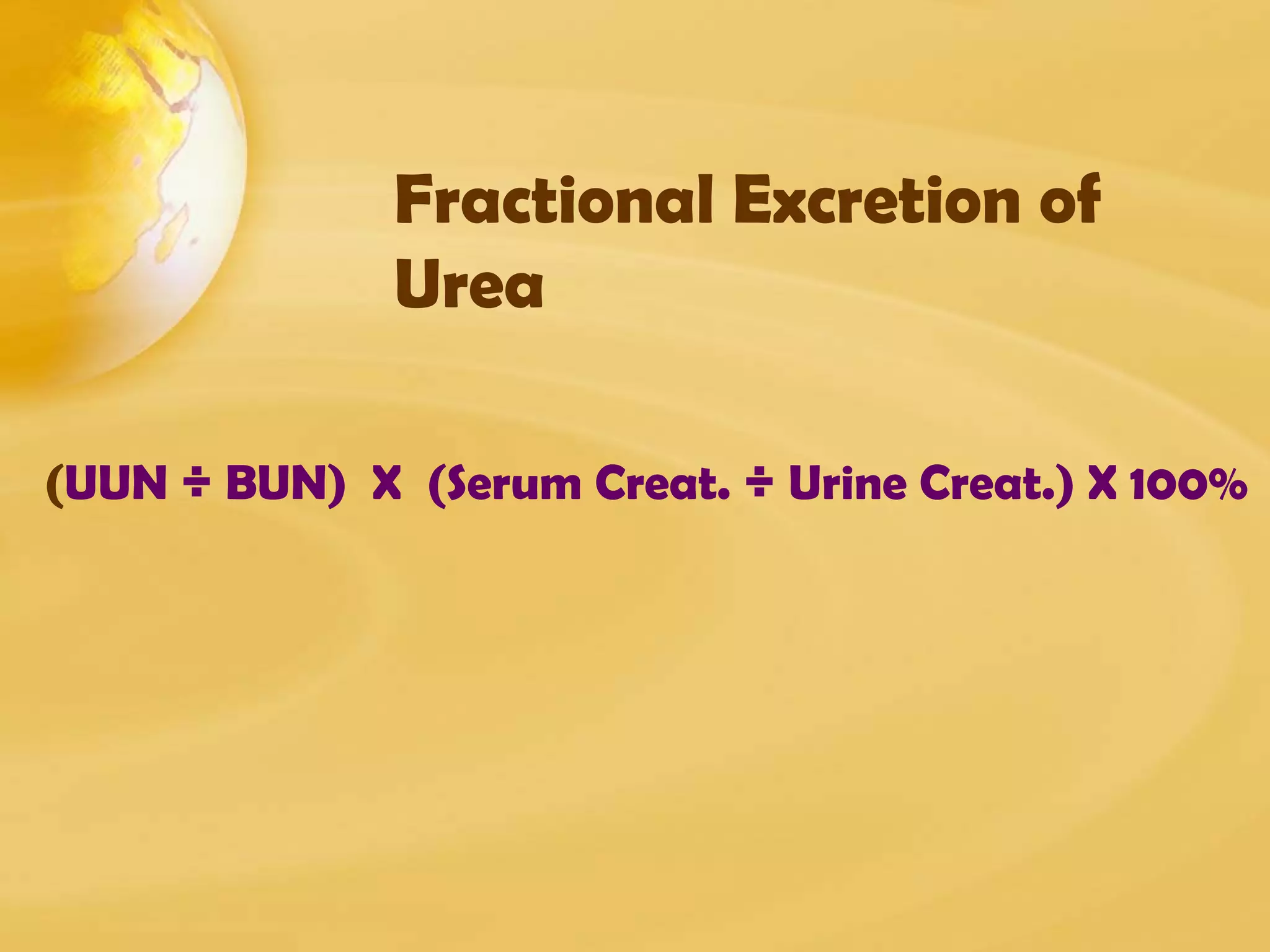
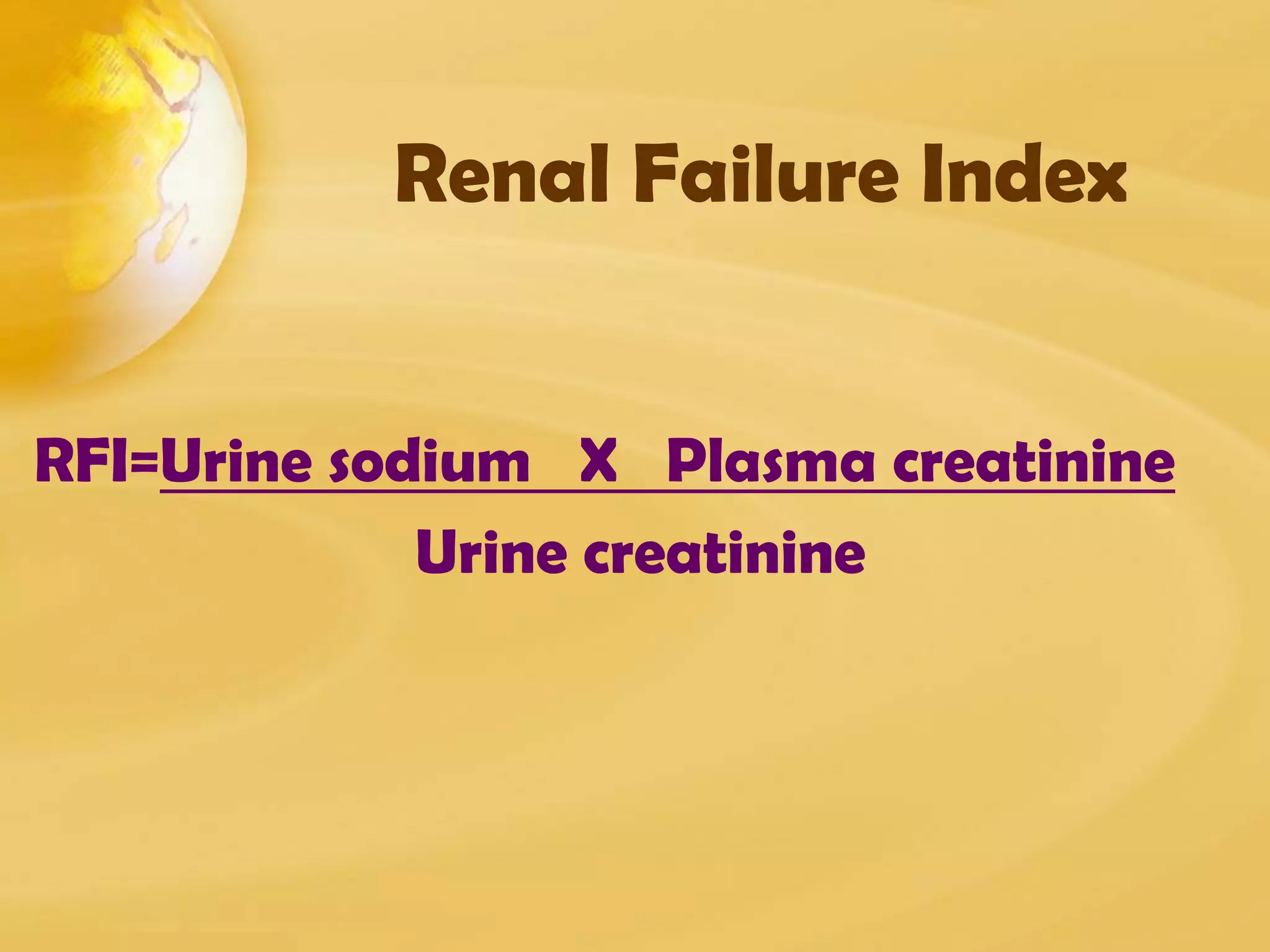
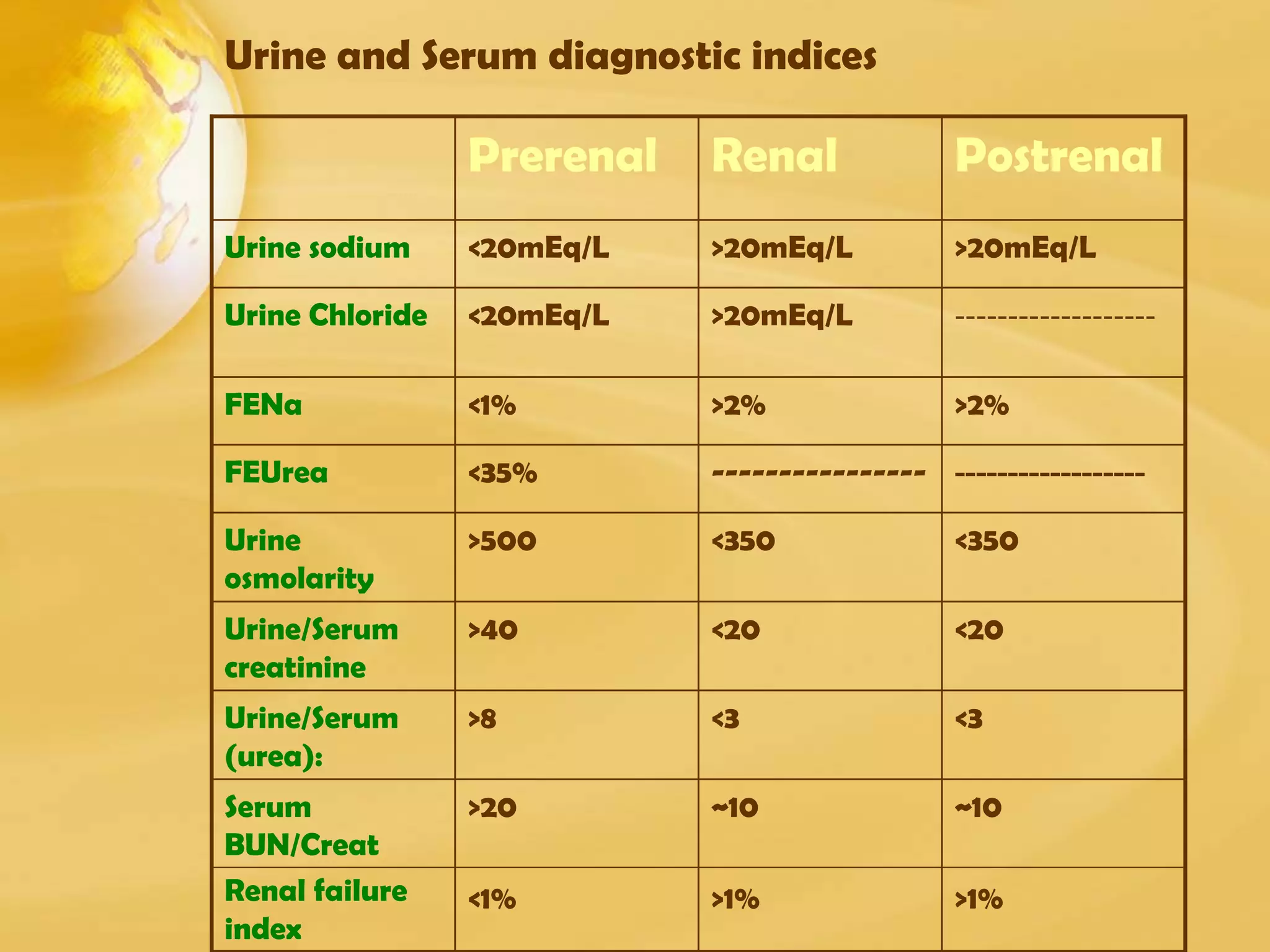
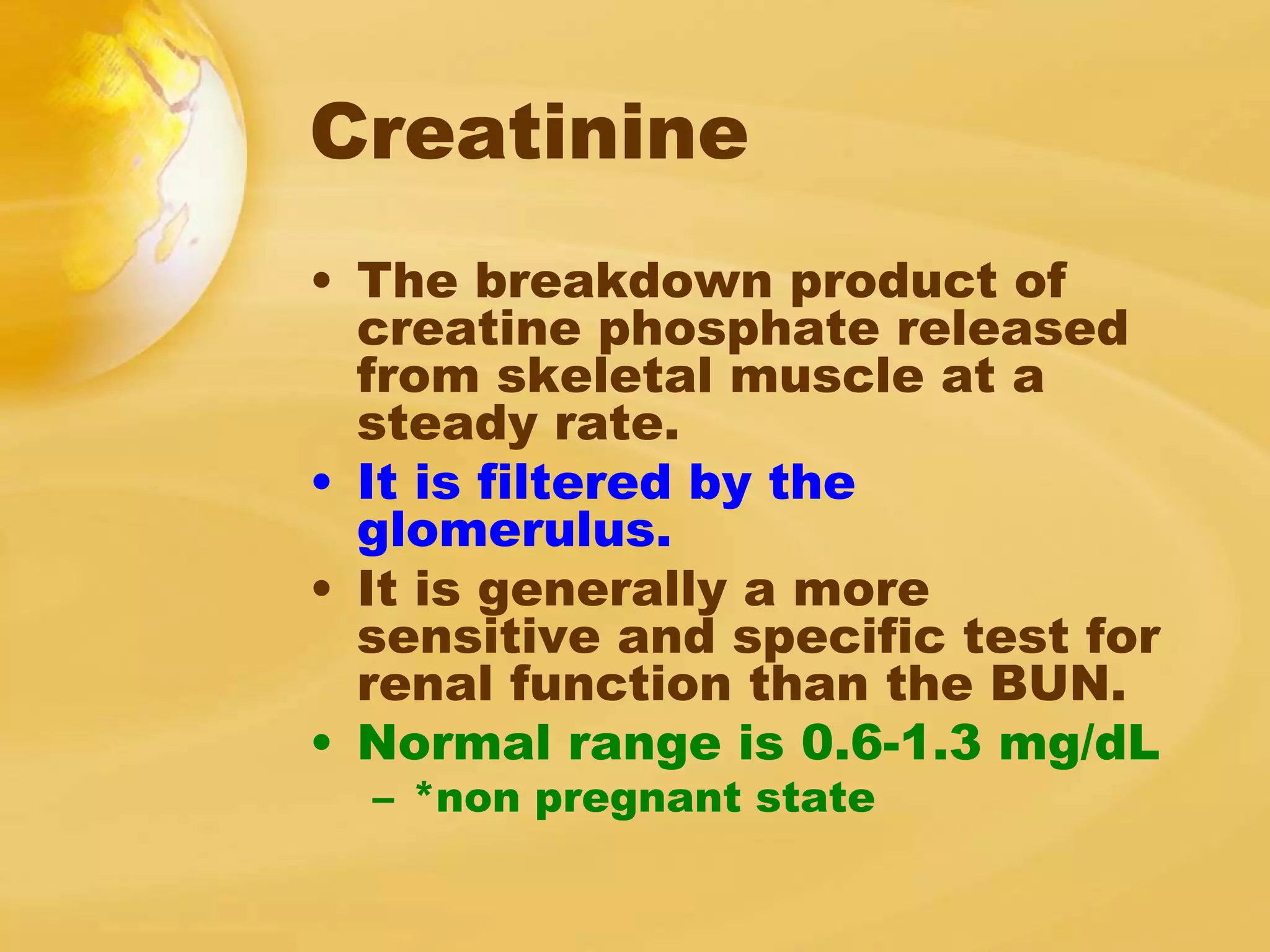
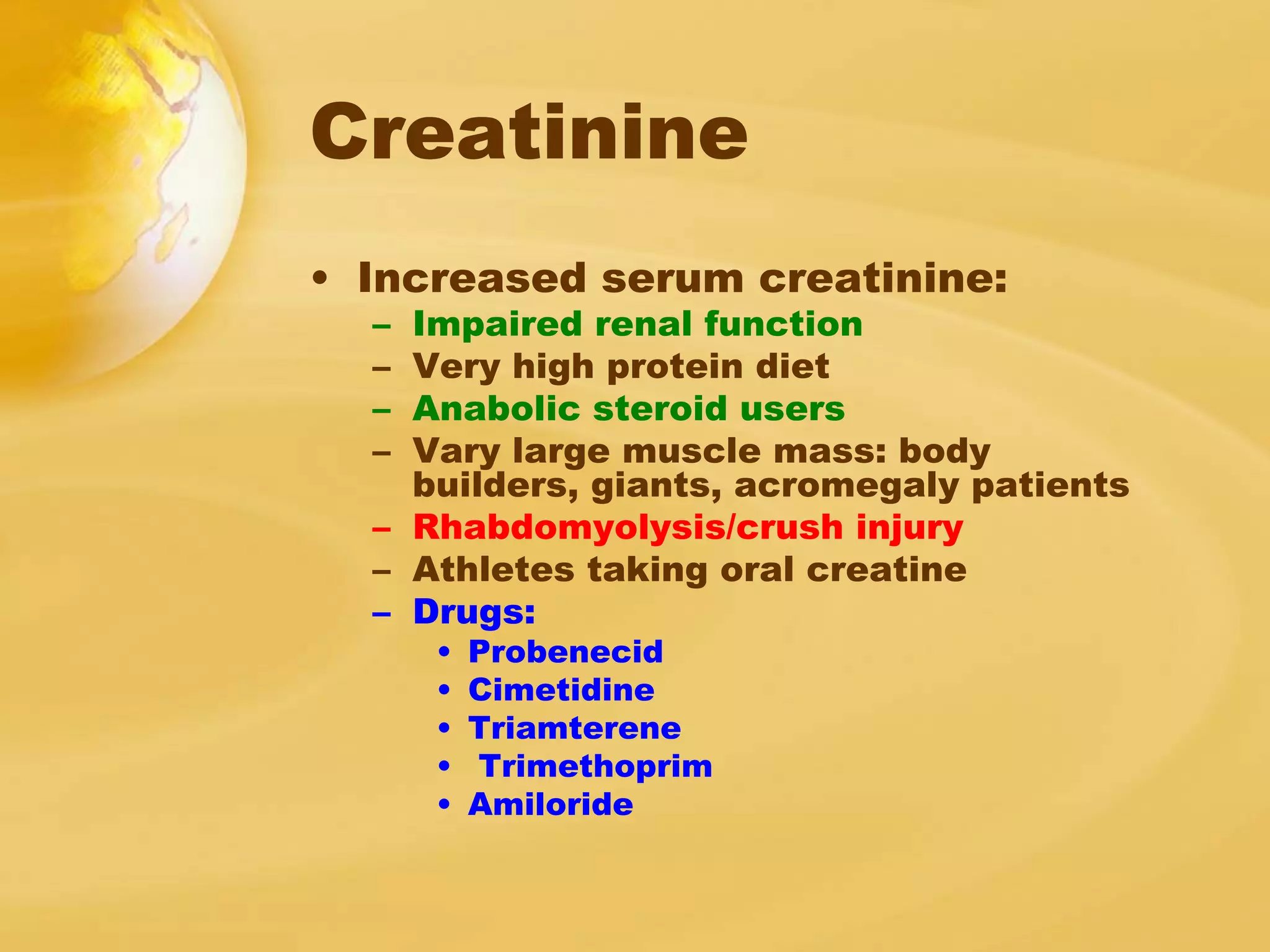
Renal function tests can help screen and monitor patients for kidney disease. The creatinine and BUN can be elevated by factors other than kidney disease, such as increased protein intake or muscle breakdown. To determine if acute renal failure is prerenal or renal (ATN), fractional excretion of sodium and urea are used, with prerenal azotemia having FENa <1% and FEUrea <35%. Estimating glomerular filtration rate (GFR) stages chronic kidney disease.

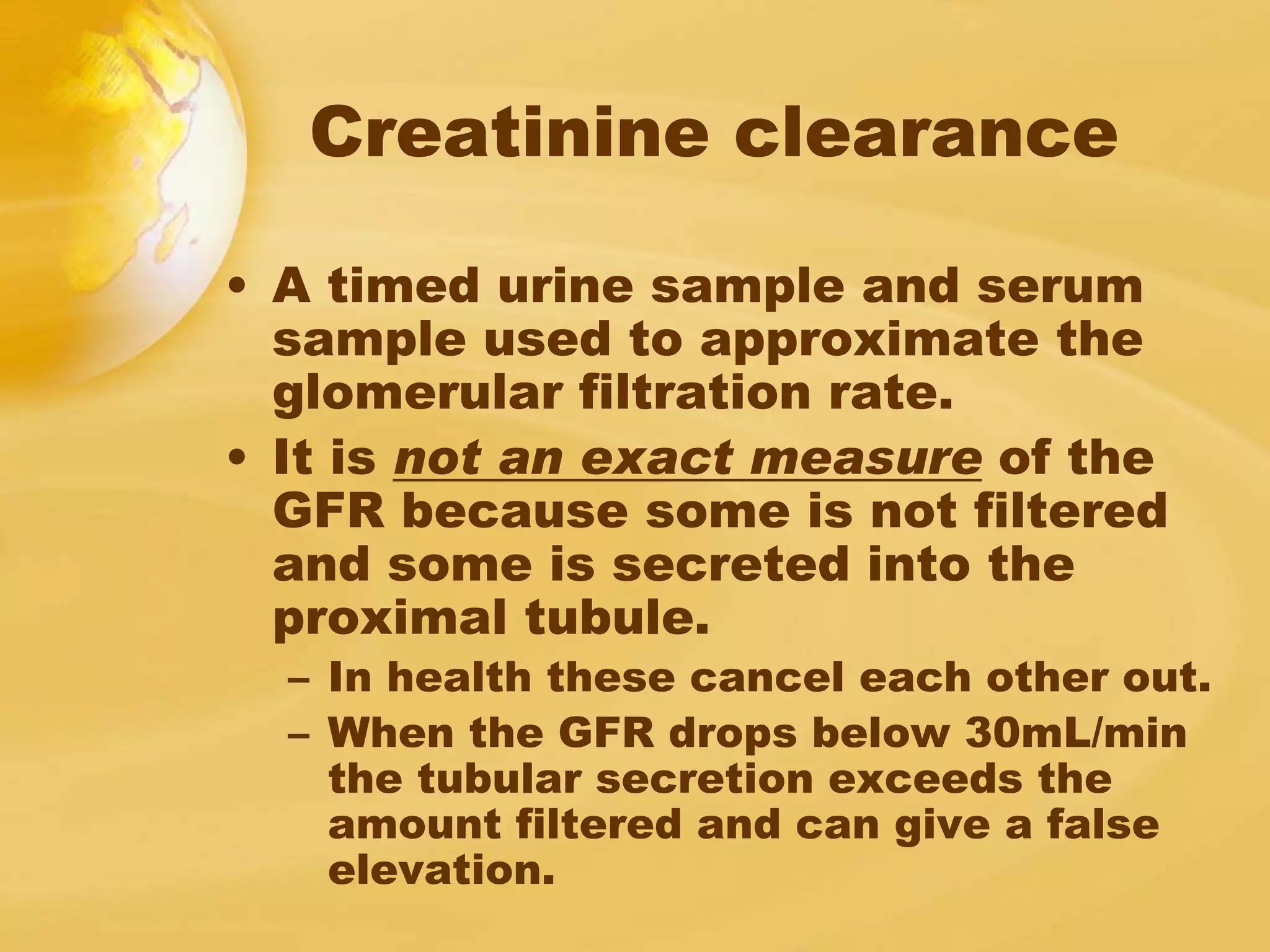
![Glomerular filtration rate: GFR
• GFR: sum of the filtration rates in all of the
functioning nephrons
GFR = [UCr x V]/PCr
**Timed collection over 24 hours
CCr = [UCr md/dL x V L/day]/ PCr mg/dL =
liter/day
*This value can be multiplied by 1000 to
convert to mL and divided by 1400 (the
number of minutes in a day) to convert into
units of mL/min](https://image.slidesharecdn.com/kidenyfunctiontest-141103130251-conversion-gate02/75/Kideny-function-test-12-2048.jpg)