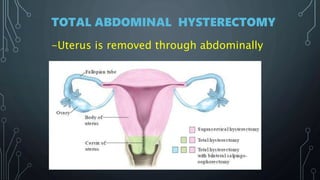
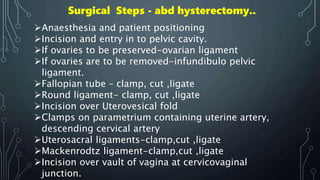
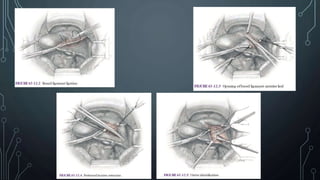
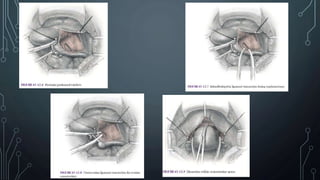
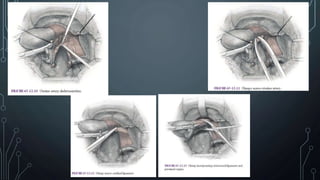
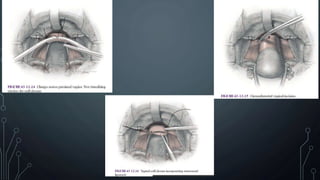
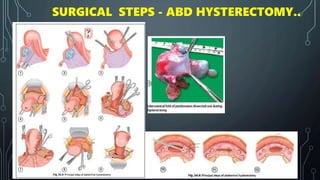
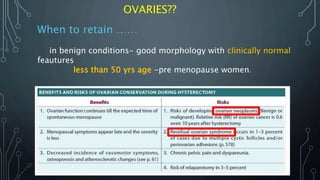
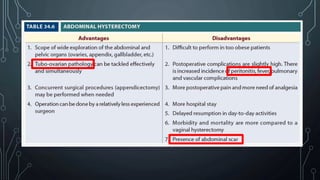
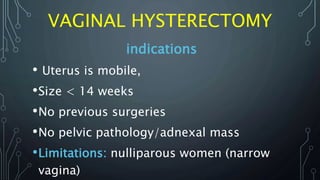
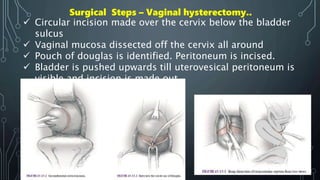
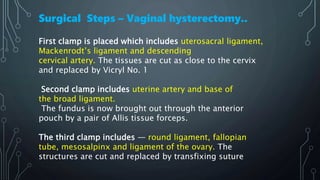
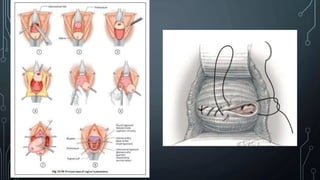
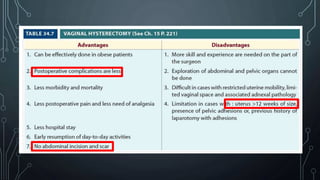
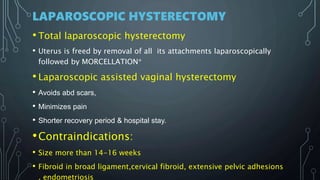
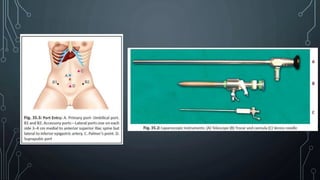
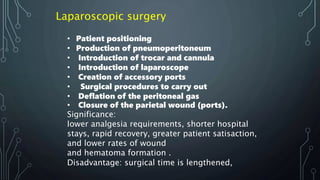
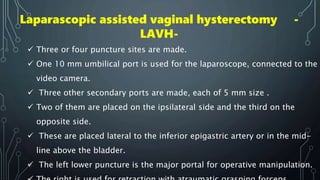
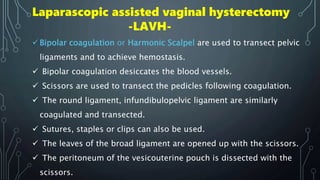
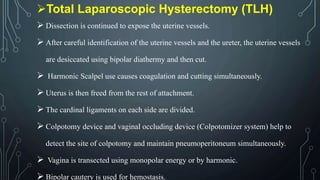
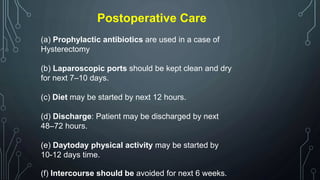
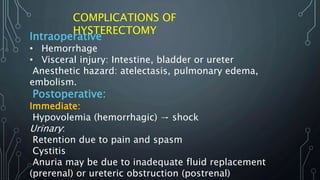
This document provides information about hysterectomy procedures for fibroids. It discusses the different types of hysterectomy including abdominal, vaginal, and laparoscopic hysterectomy. Indications for hysterectomy in fibroids include age over 40, failure of medical treatment, large fibroid size, and complications from prior procedures. The steps for each hysterectomy procedure are outlined. Complications can include hemorrhage, visceral injury, urinary issues, and late complications such as incontinence or infection. In summary, this document reviews hysterectomy as a treatment for fibroids, compares different surgical approaches, and lists indications and complications.