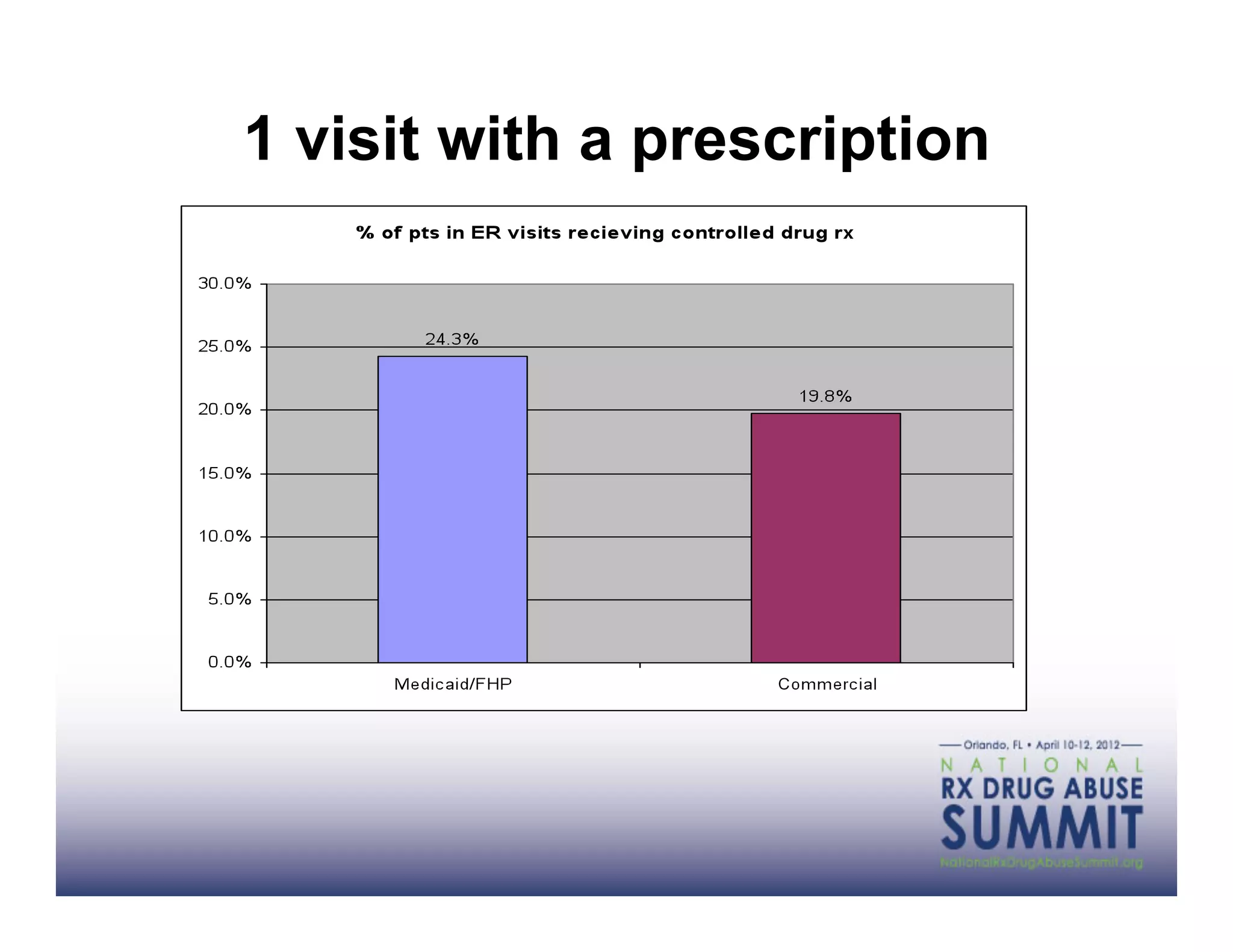
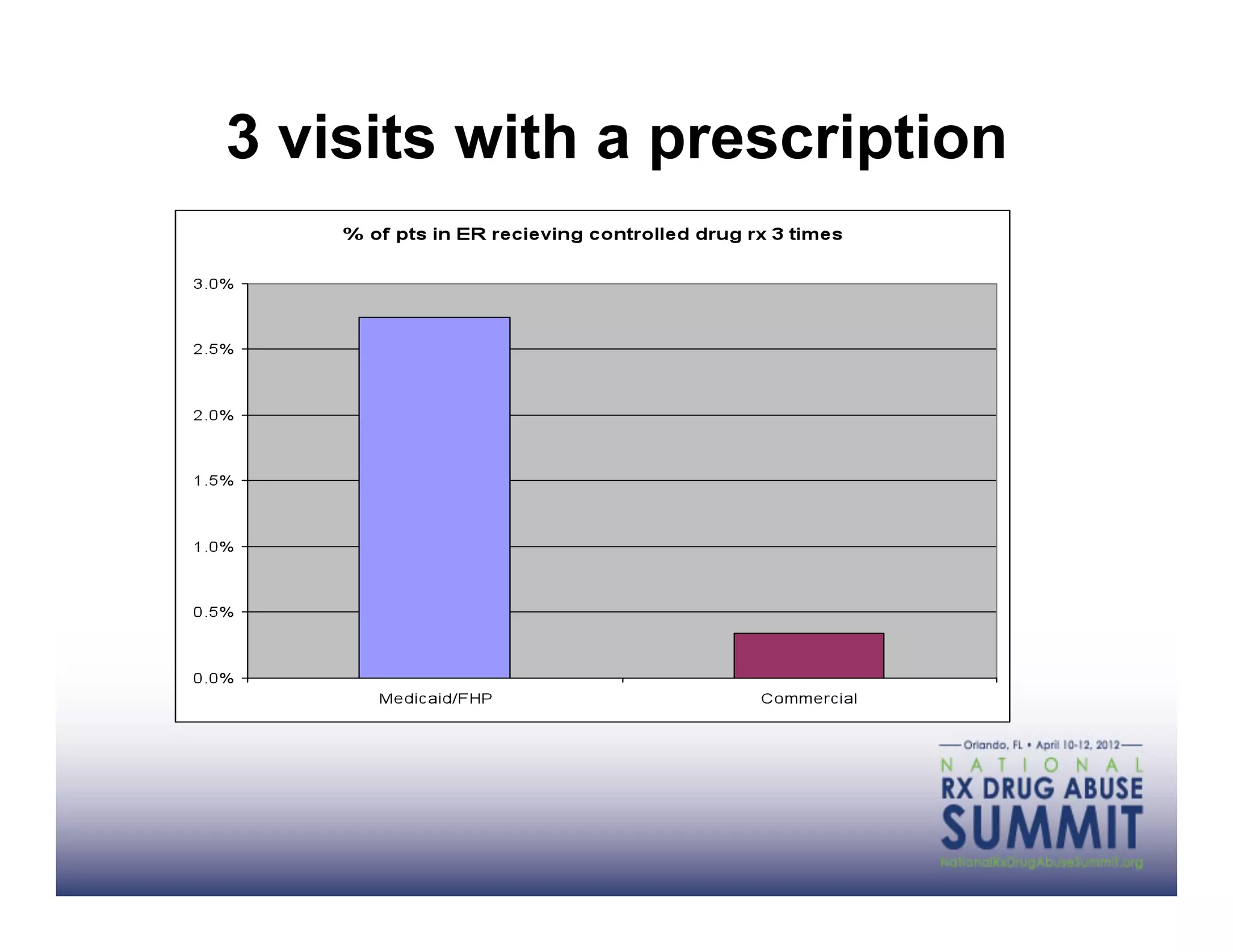
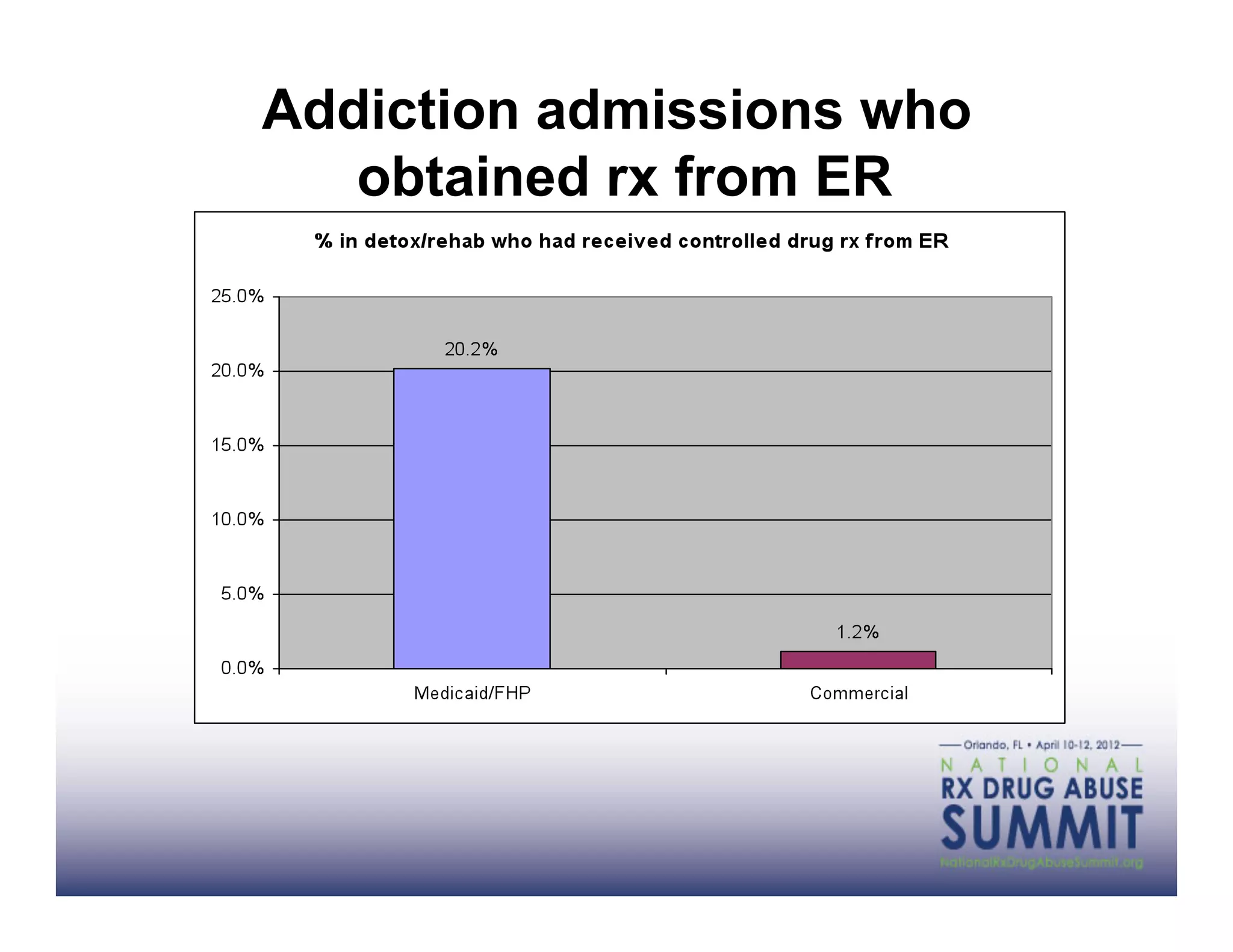
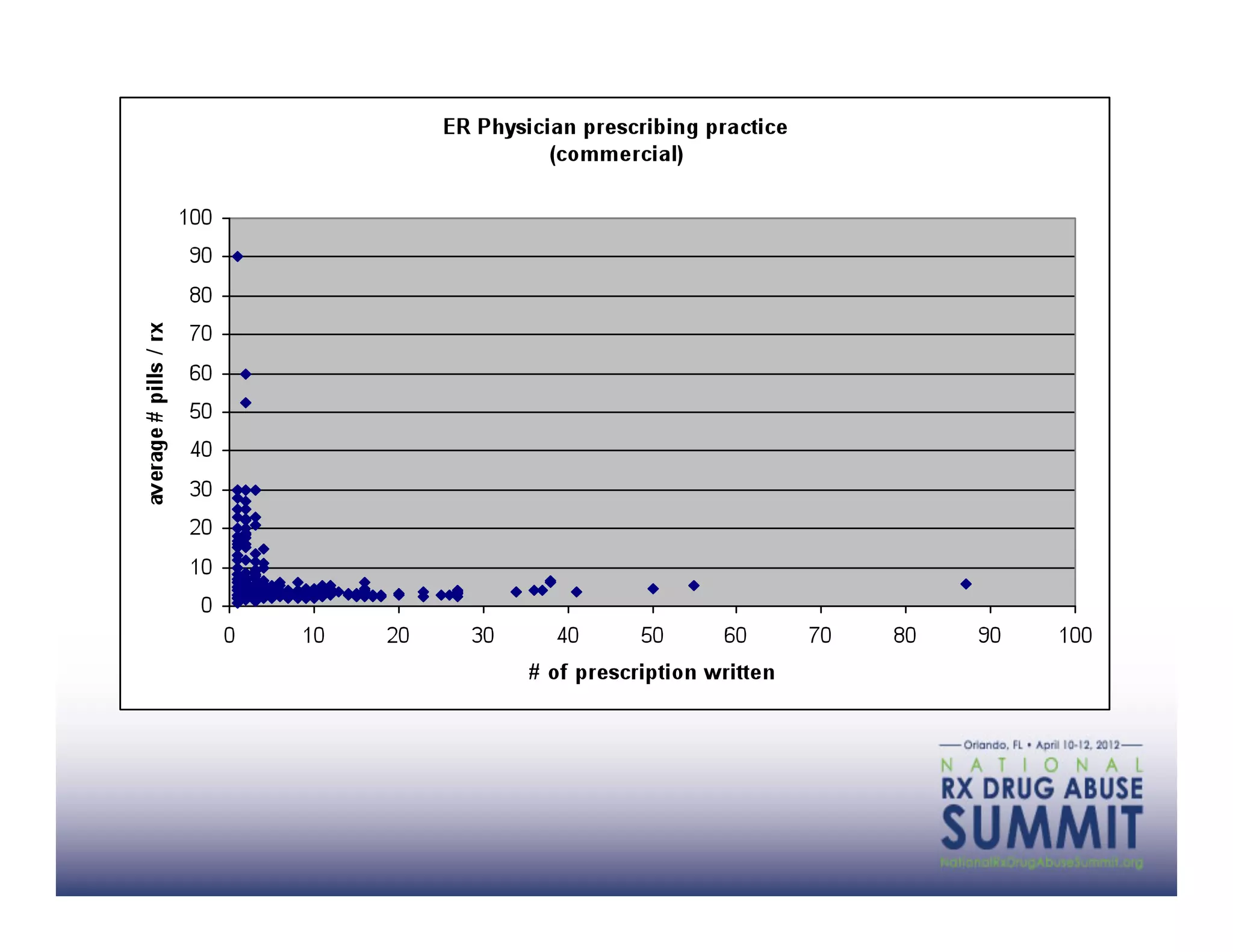
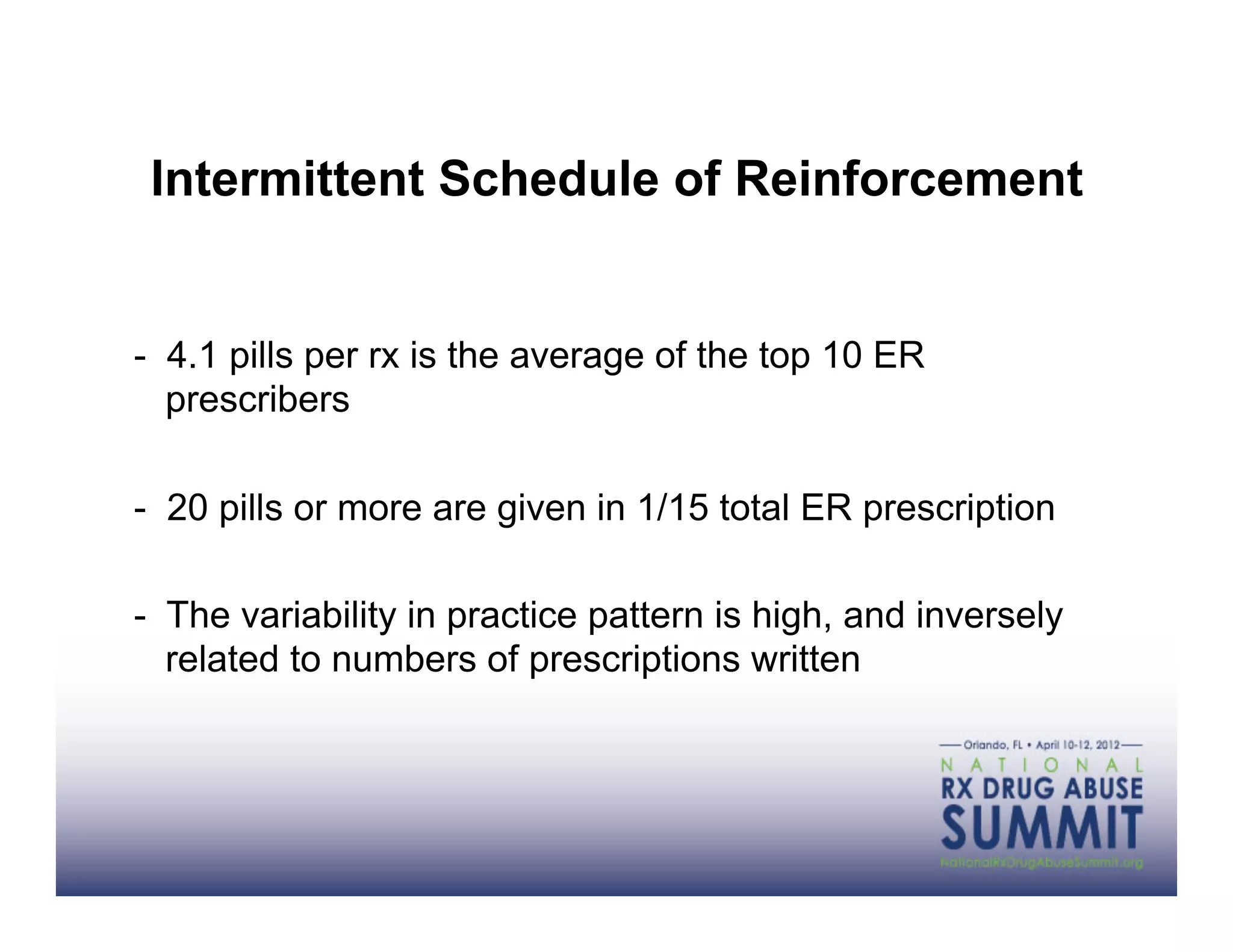
This document discusses opioid dependence issues faced by health plans and strategies to address them. It identifies barriers to responsible pain management like lack of provider information, skills, and external incentives. Health plans have data on total costs across settings that can identify population problems and inform practices. Strategies for health plans include using data to educate providers, changing policies, and working with providers on care coordination, prior approvals, pharmacy management, and innovative payment models. The best approaches coordinate objective patient information, expert collaboration, and payment reform focused on total cost of care.