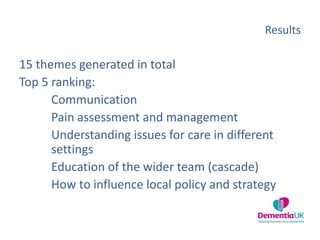
The document describes the establishment of a Community of Practice (CoP) between Dementia UK and Hospice UK to improve end of life care for those with dementia. Over 700,000 people in England live with dementia, yet they often receive poor end of life care and are more likely to die in hospitals than hospices. The inaugural CoP meeting used a prioritization technique to identify key issues: communication, pain management, care across settings, educating staff, and influencing local policy. Since then, the CoP has grown to 180 members, published articles, and plans further knowledge sharing activities and evaluation to improve dementia end of life care.



![Communication
“.…difficult conversations….how to communicate.…for the
distressed person with dementia who is unable to cooperate…”
“….not straight forward [in dementia]….everyone is different….”
“….not just communication with the person with dementia but
their carer too….”](https://image.slidesharecdn.com/karenharrison-161117094338/85/Karen-Harrison-10-320.jpg)
![Pain assessment & management
“.…[need]….to understand how to assess and manage pain….”
“….pain management should be a part of care management for
distress behaviours….”
“….pain education….not just seeing agitation and treating
agitation….”](https://image.slidesharecdn.com/karenharrison-161117094338/85/Karen-Harrison-11-320.jpg)
![Dementia care in different settings
“.…there needs to be a shared ethos between hospices and care
homes….and what each can offer….”
“….do we have enough staff….do people with dementia need
more staff [to care for them]….”](https://image.slidesharecdn.com/karenharrison-161117094338/85/Karen-Harrison-12-320.jpg)
![Educating the wider team
“.…we each know what we know but how do we get to know
what we don’t know….?”
“….[more people with dementia]….are expected to come to our
hospice but how can I support the staff educational needs when I
am not an expert in this….?”](https://image.slidesharecdn.com/karenharrison-161117094338/85/Karen-Harrison-13-320.jpg)
![Influencing local policy and strategy
“….[I want to understand]….ways to get management, clinical
commissioning groups on board….”
“….[I want]…. training in effective business case
preparation….[making a case for people with dementia to access
hospice]….”
“….[I]….would like dementia to be a seriously funded and thought
about as cancer….”](https://image.slidesharecdn.com/karenharrison-161117094338/85/Karen-Harrison-14-320.jpg)