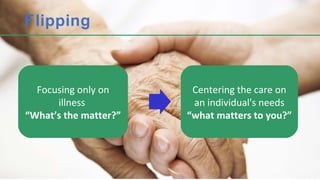
The document discusses supporting people with dementia in hospital settings. It aims to change perceptions of behaviors in dementia patients, challenge existing hospital systems to be more patient-focused, and identify resources to help dementia patients during hospital admissions. Specific challenges in caring for dementia patients in hospitals are outlined, including how the environment can increase confusion and distress. The language used to describe dementia and behaviors is also addressed.