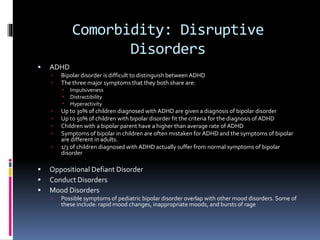
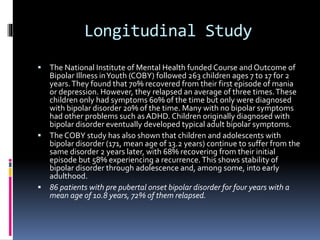
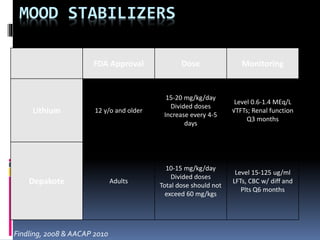
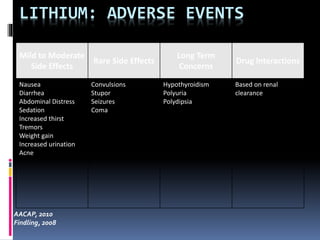
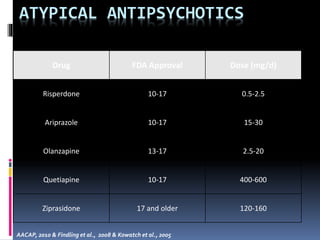
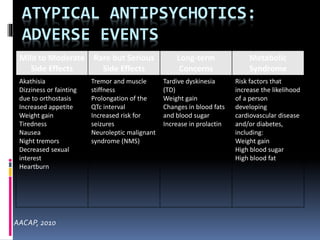
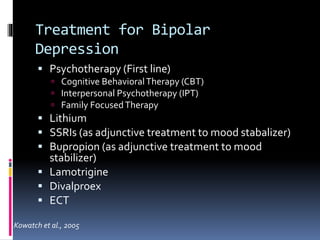
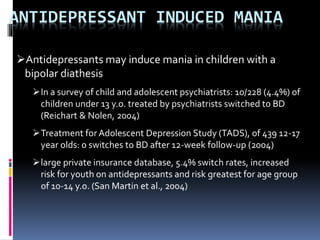
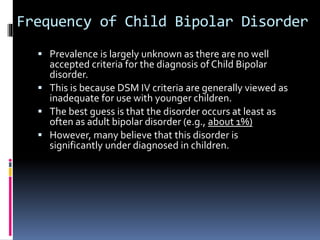
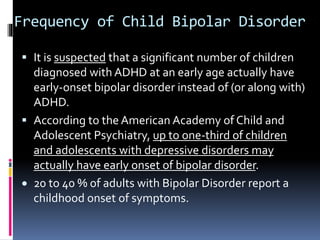
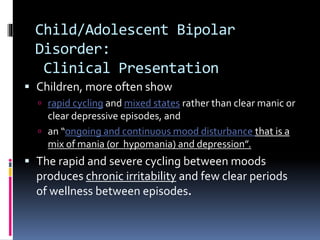
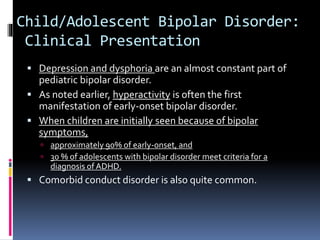
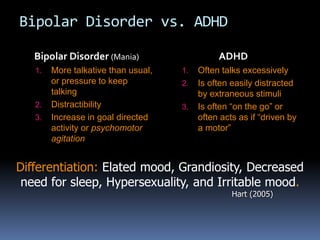
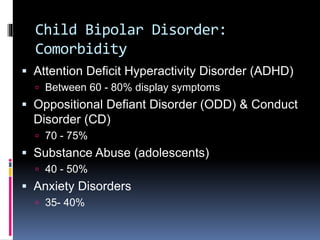
The document discusses bipolar disorder in children and adolescents. It notes that the presentation of bipolar disorder can be different in children compared to adults, with symptoms often overlapping with other disorders like ADHD. Children may experience more mixed states and rapid cycling between moods. Treatment involves mood stabilizers and atypical antipsychotics, though their use requires monitoring side effects. The prognosis is often one of recovery from initial episodes but high rates of relapse.