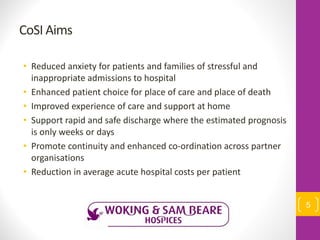
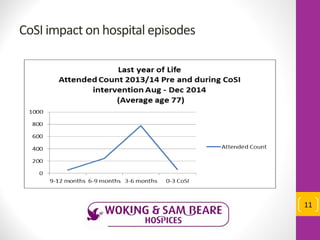
The document summarizes a palliative and end of life care service called Coordinated, Safe and Integrated (CoSI) care. CoSI aims to [1] reduce hospital admissions and support patient choice for place of care and death, [2] provide enhanced coordination of care across partner organizations for patients with 6-8 weeks to live, and [3] lower costs compared to usual care. Since launching in 2014, CoSI has supported over 500 patients, with 76% receiving care within 48 hours and 100% of patients who died achieving their preferred place of death at home. Evaluation found acute care costs were £1,700 on average for CoSI patients versus £3,812 for others in their last 3 months