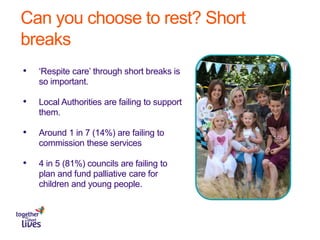
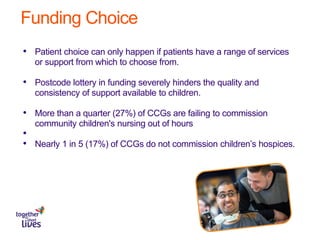
This document discusses the need for choice and patient-centered care in children's palliative care. It notes that there are approximately 49,000 children in the UK with life-limiting conditions, yet their voices are often not heard and patient choice is absent. Parents describe the system as a "minefield" with a lack of support and coordination. Short breaks for respite care are important but often not funded by local authorities. Choice is limited by a lack of services due to underfunding. The document calls for improved coordination, a national inquiry, mandated joint commissioning, and greater transparency and accountability in funding to better meet the needs of children requiring palliative care and their families.