This document discusses nutritional anemia, its causes, prevention, and control in India. It provides the following key points:
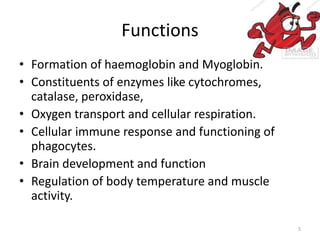
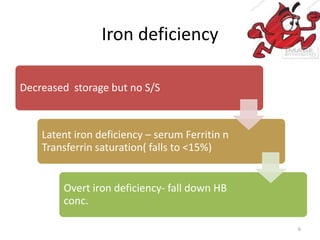
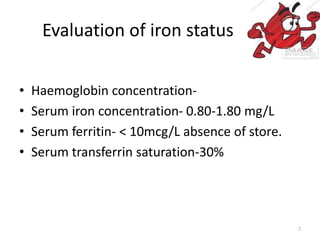
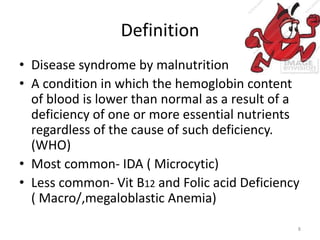
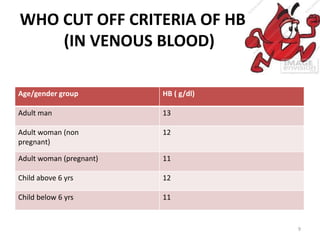
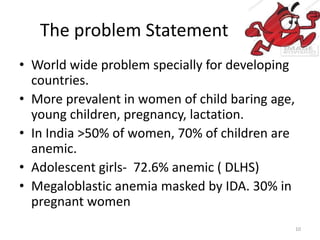
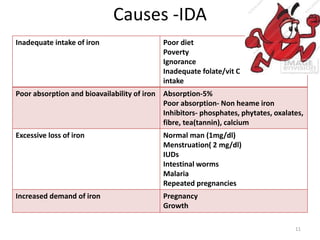
1. Nutritional anemia is caused by a deficiency of iron and/or other nutrients like folate and vitamin B12, and is the most common form of anemia globally and in India.
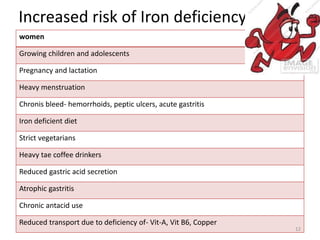
2. Risk groups for iron deficiency anemia in India include women of childbearing age, young children, pregnant women, and adolescents. Over 50% of women and 70% of children in India are estimated to be anemic.
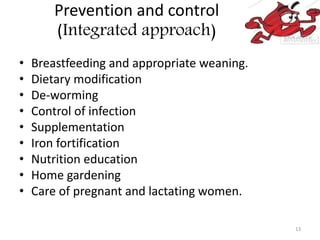
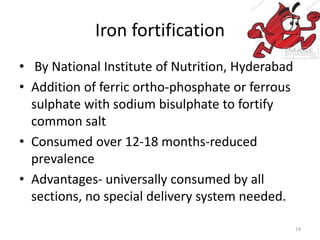
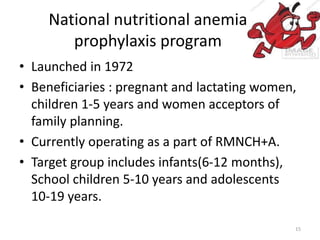
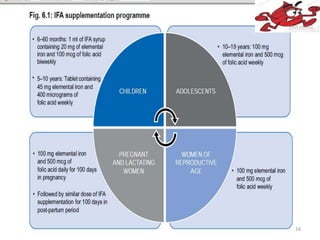
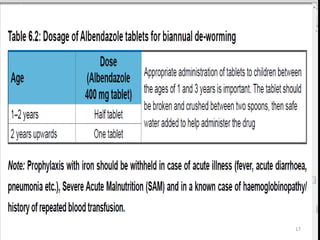
3. Prevention strategies in India include iron fortification of foods like salt, supplementation programs that provide iron and folic acid to at-risk groups