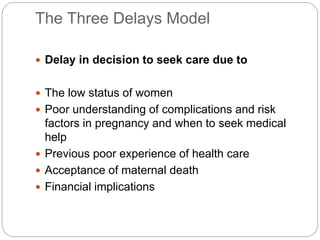
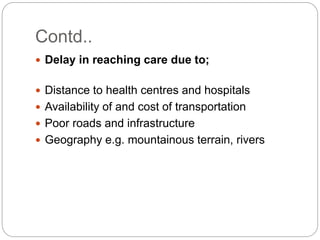
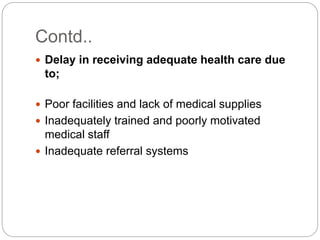
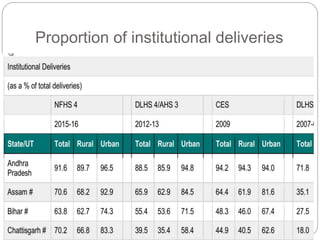
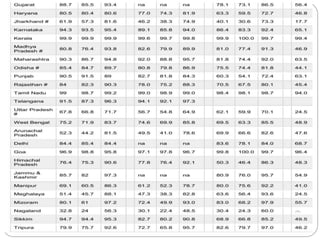
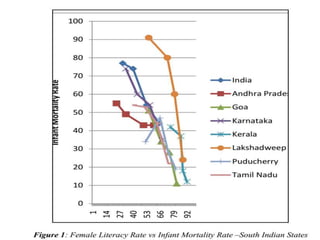
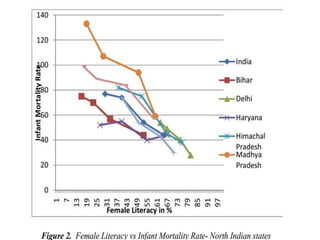
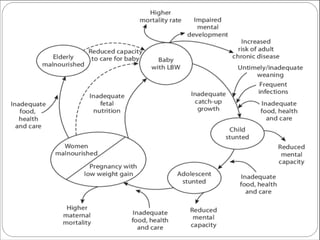
This document discusses social obstetrics, which examines the relationship between social factors and human reproduction. It deals with topics like age at marriage, fertility patterns, education levels, and a woman's role in society. Social obstetrics considers these environmental influences in addition to medical skills. It evolved from concepts introduced by WHO in 1966 and aims to treat patients as members of families and communities. Barriers like lack of education, financial issues, and infrastructure can delay women's decisions to seek care, ability to reach care, and receipt of adequate care. Improving factors like female literacy are associated with reduced maternal and infant mortality. Training emphasizes delivering integrated maternal and child health/family planning services in rural communities.