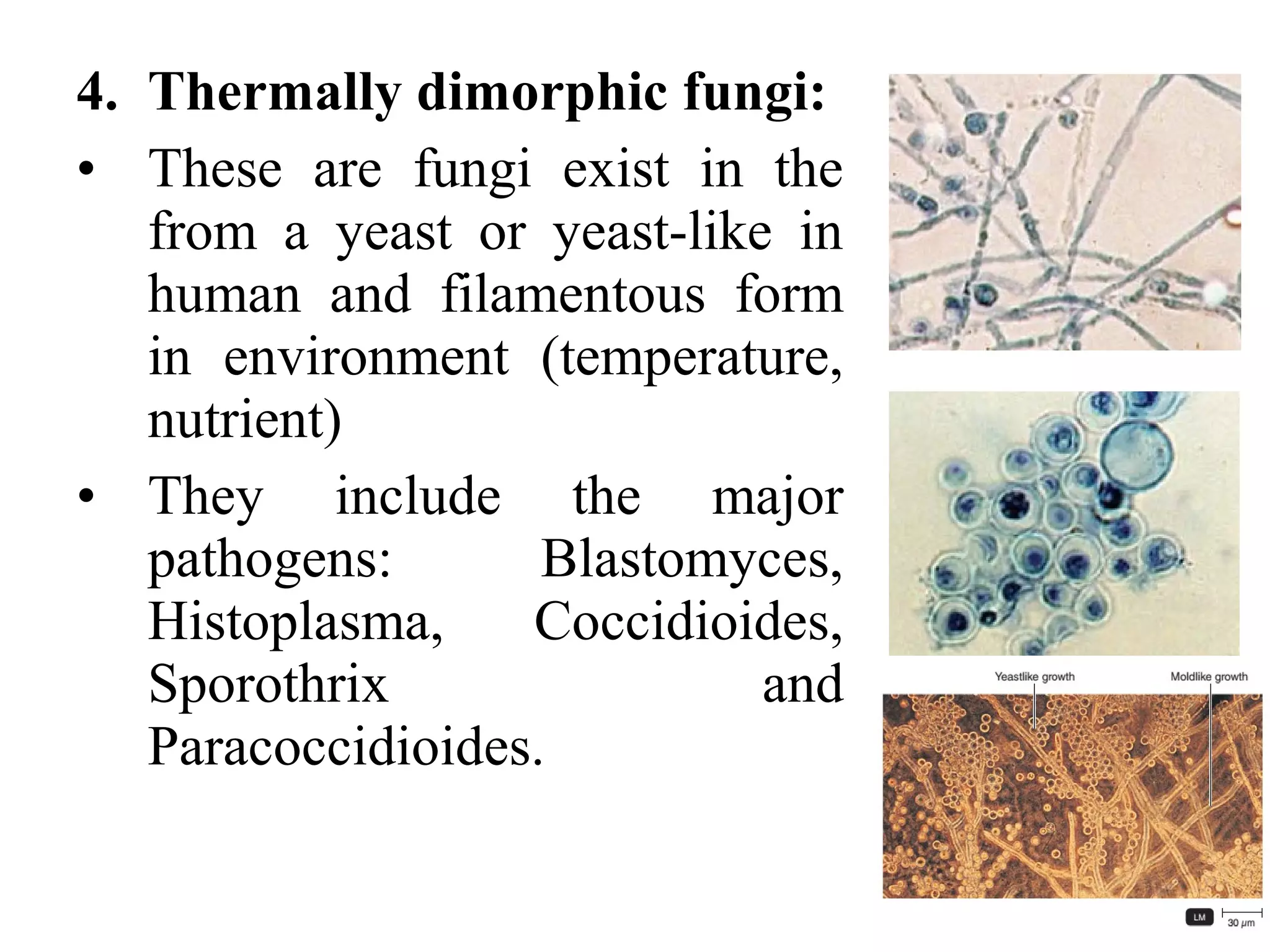
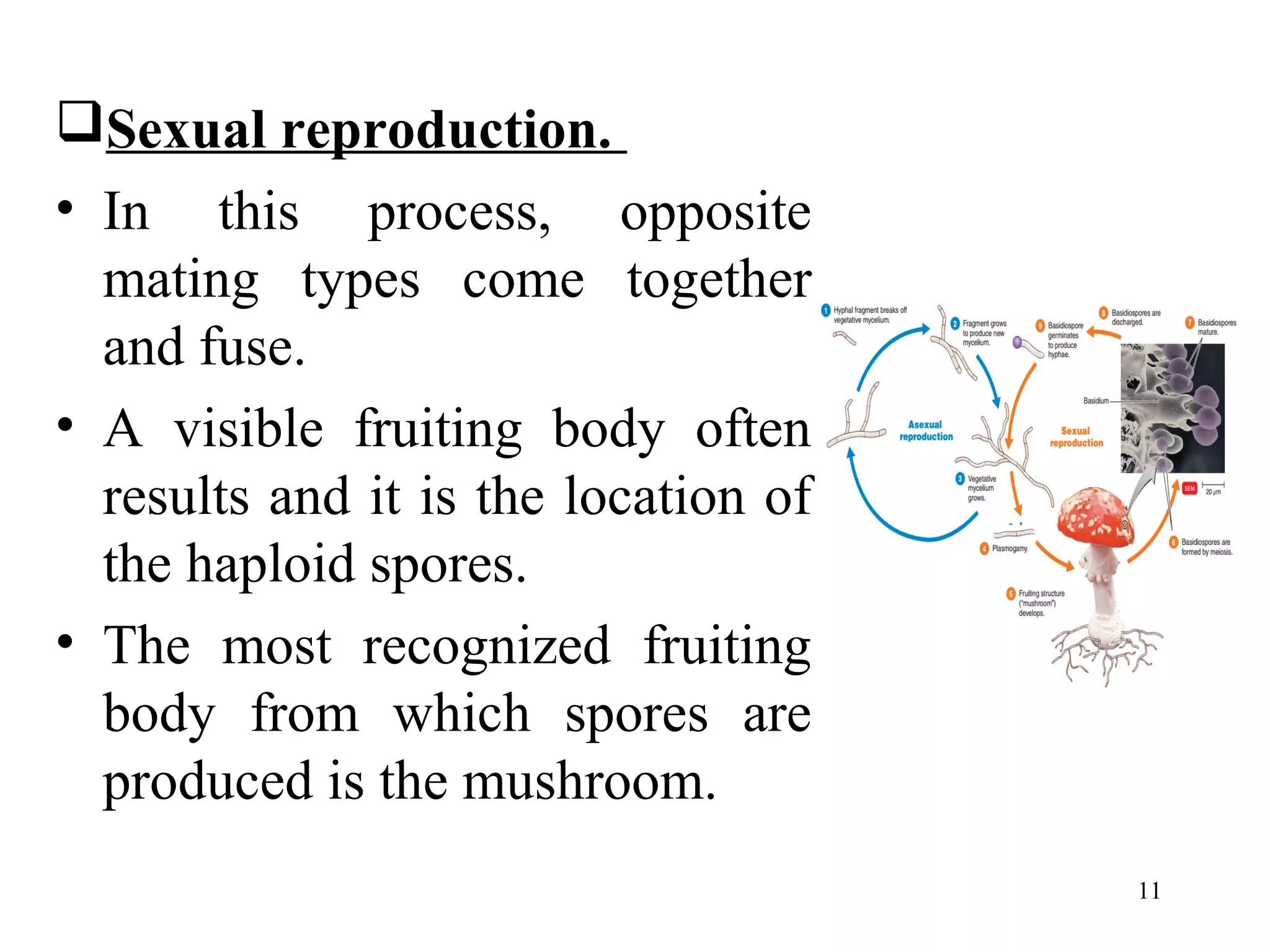
This document discusses fungi as infectious agents. It describes the structure of fungi including hyphae, yeasts, pseudohyphae, and thermally dimorphic fungi. It covers fungal reproduction through both sexual and asexual means. The document also discusses fungal nutrition, disease pathogenesis, diagnosis of fungal infections, and control of fungal infections.