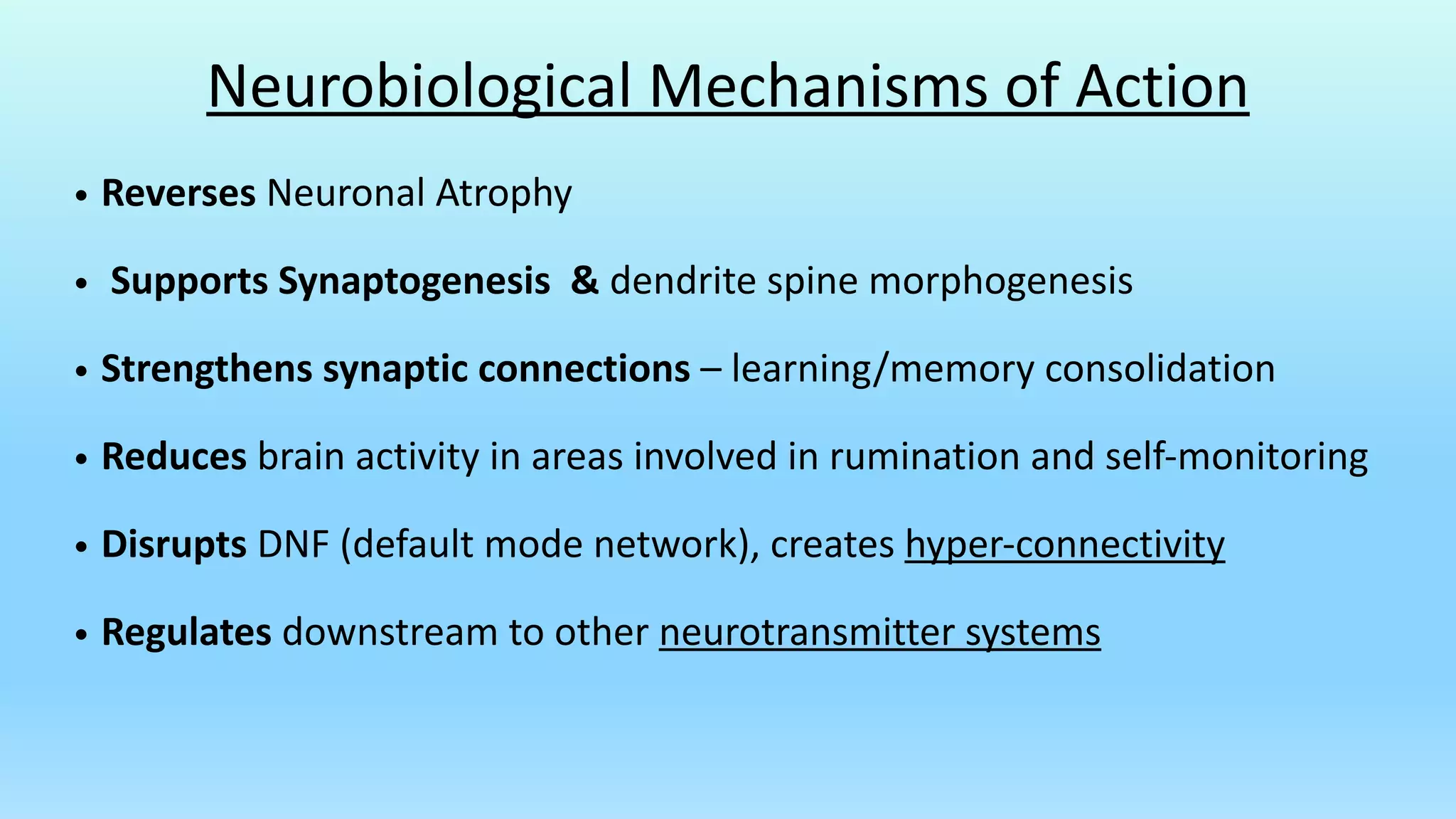
The document is an overview of ketamine-assisted psychotherapy, detailing its history, mechanisms, therapeutic applications, and treatment protocols. It covers treatment indications for various mental health conditions, the psychotherapeutic model employed, and potential risks and contraindications. The document highlights the importance of collaborative treatment planning and integration of experiences for effective patient outcomes.