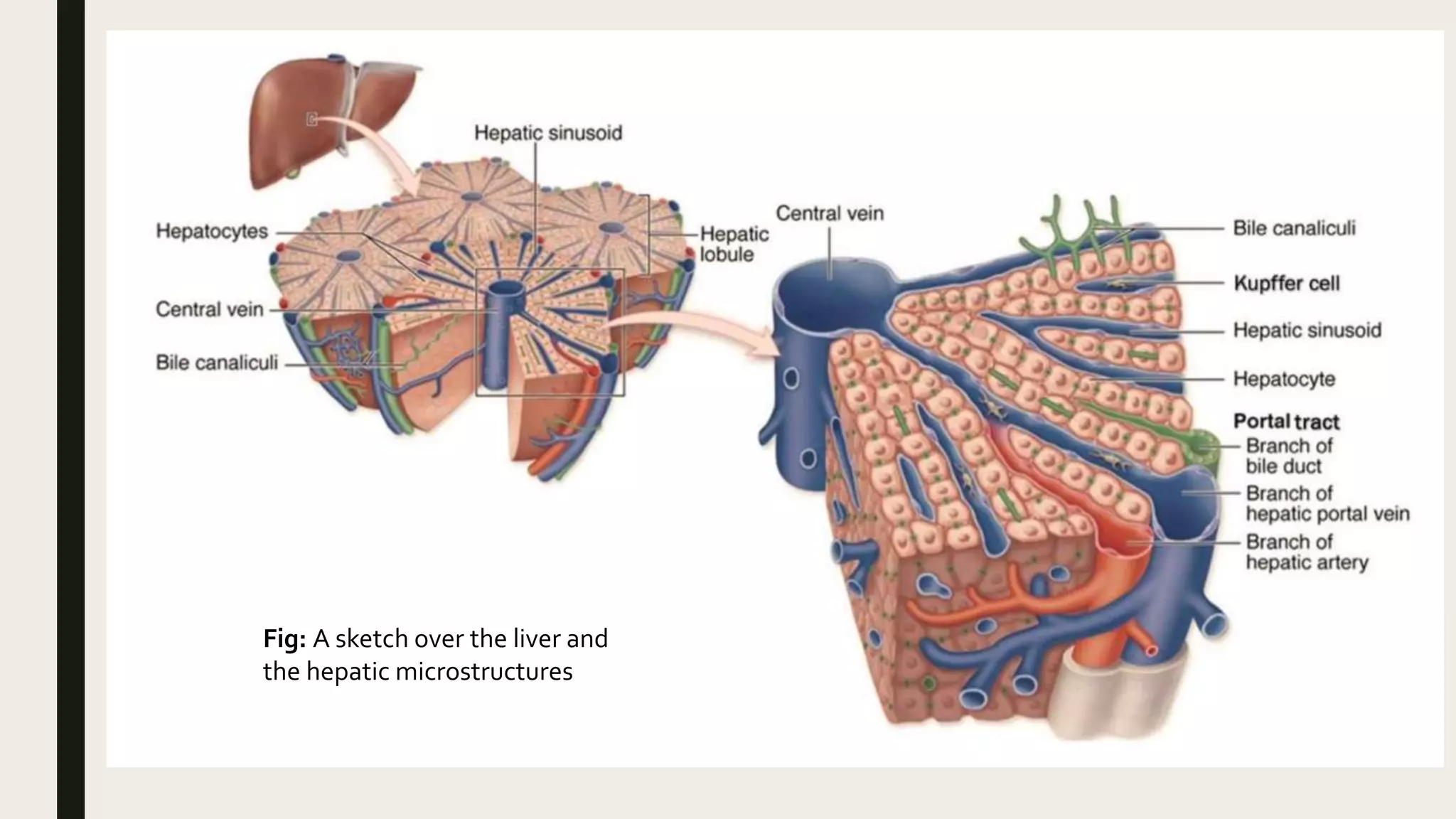
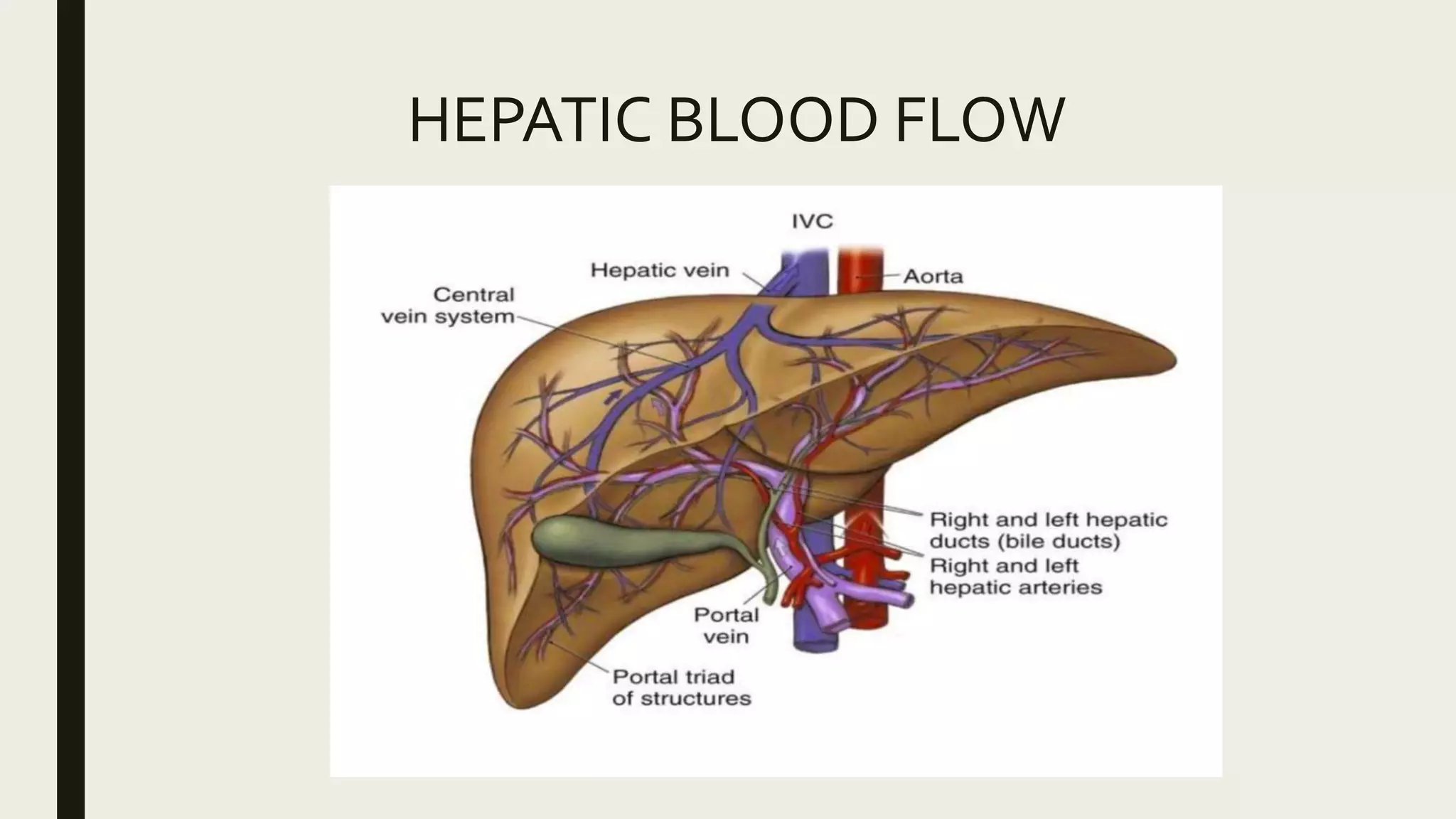
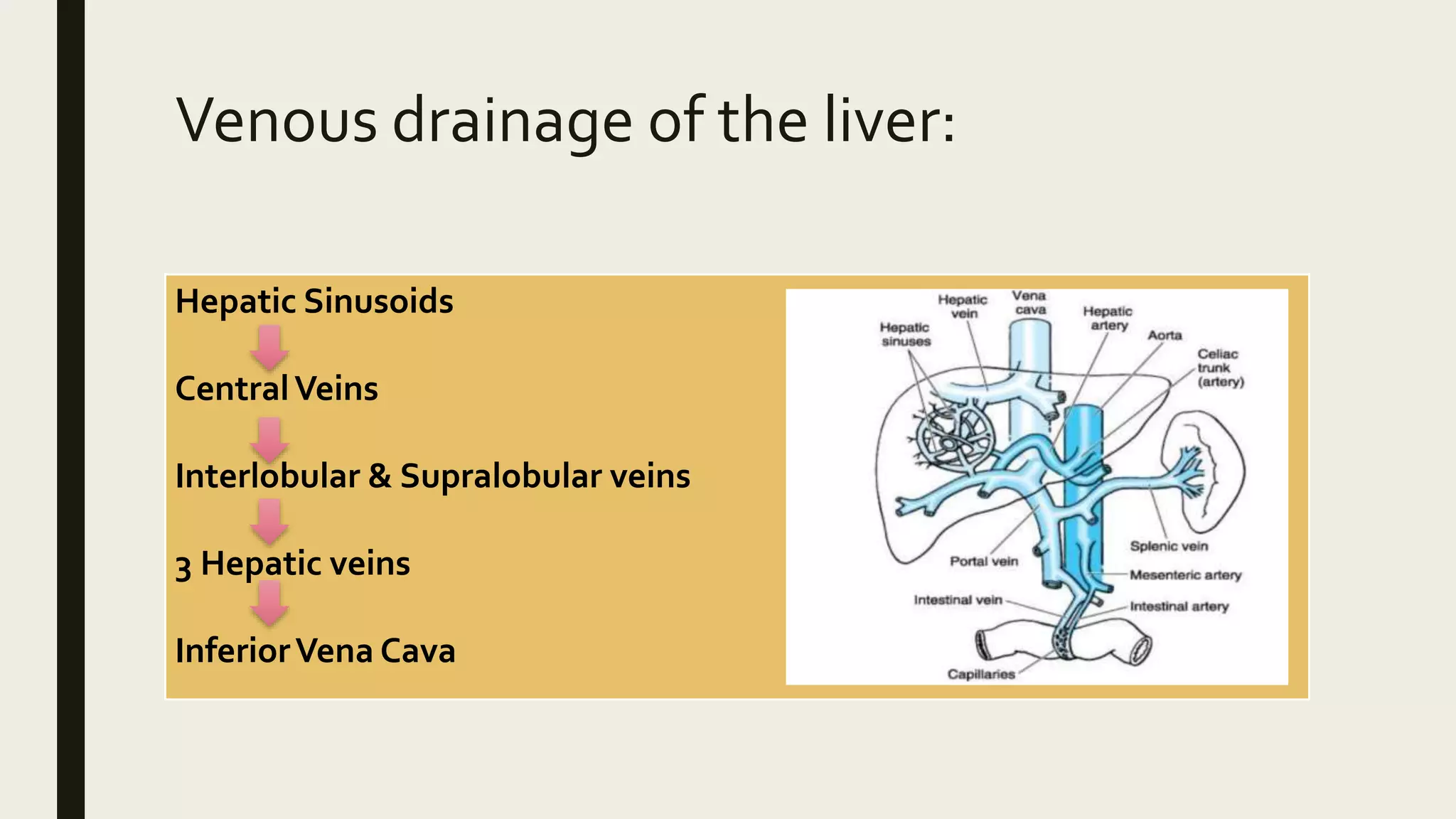
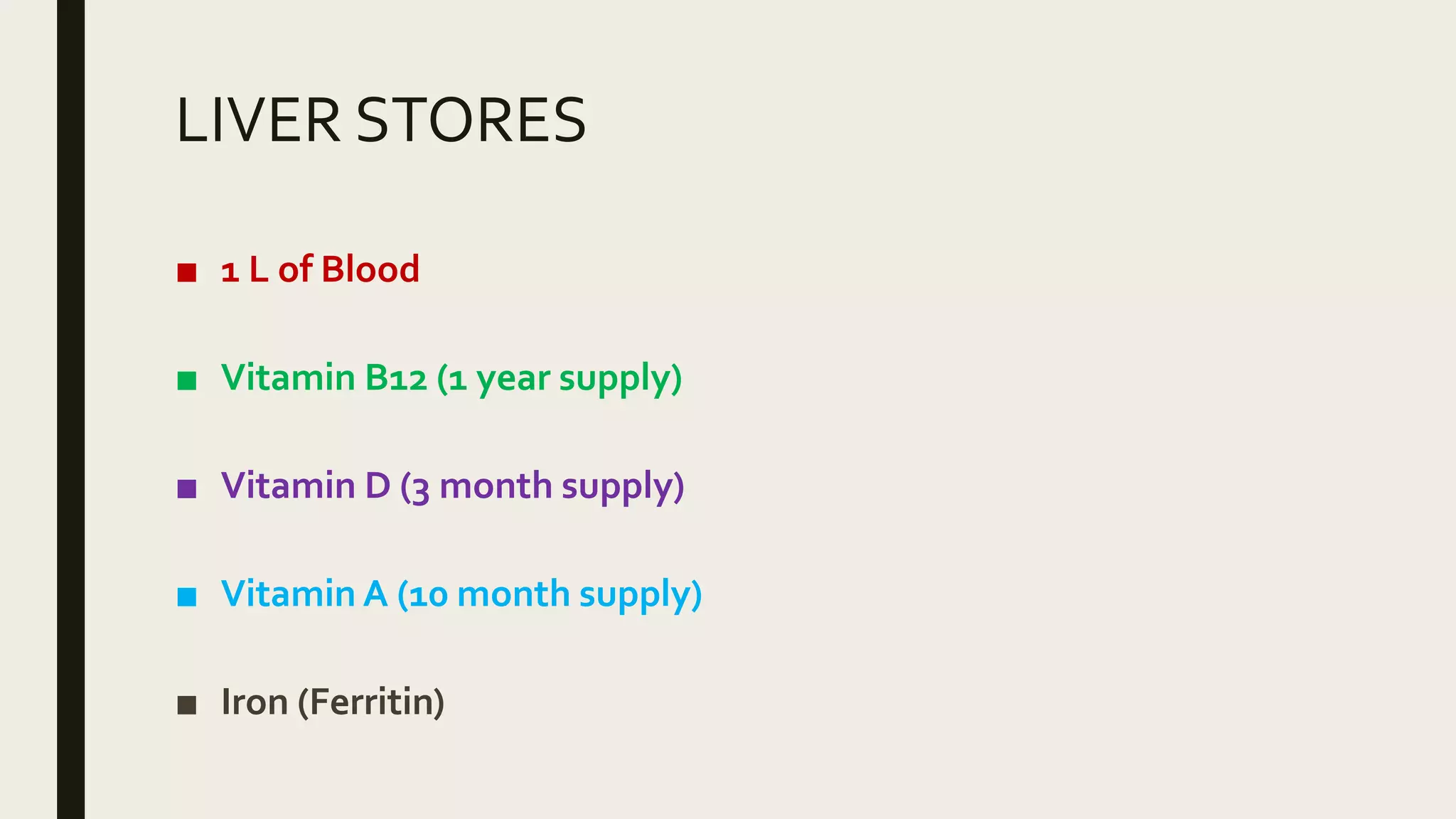
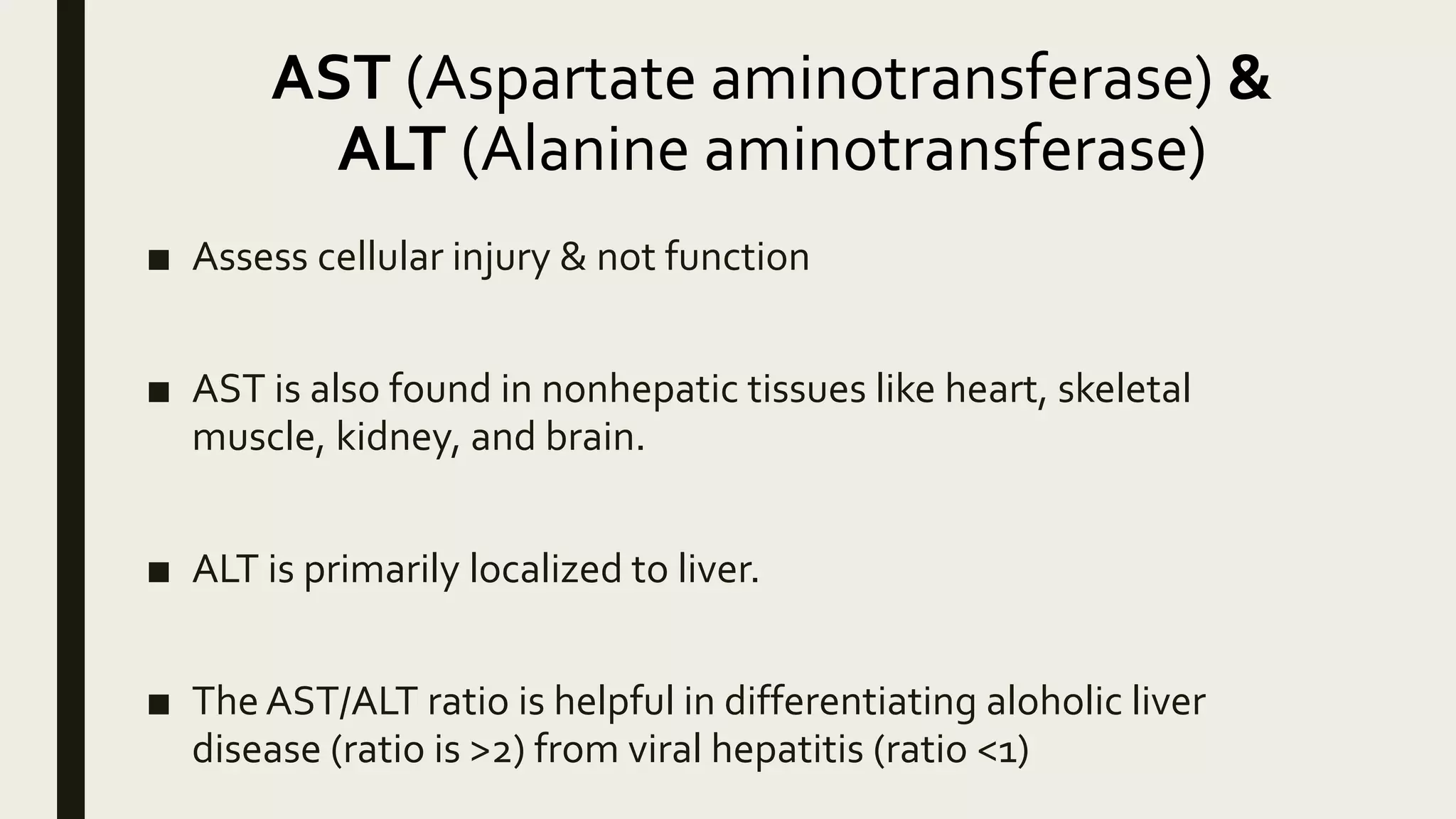
The liver performs many essential functions including metabolism, synthesis of proteins and clotting factors, and storage of vitamins and minerals. It receives approximately 1.5 L of blood per minute, regulated through intrinsic and extrinsic mechanisms. The basic structural and functional unit of the liver is the lobule, containing hepatocytes arranged in plates around a central vein. Anaesthetic agents can impact hepatic blood flow and metabolism. Tests of liver function include albumin and clotting factors to assess synthesis, and AST, ALT, alkaline phosphatase and bilirubin to detect cellular injury.