The document summarizes the structure and function of the integumentary system in 3 paragraphs:
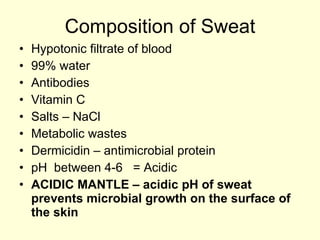
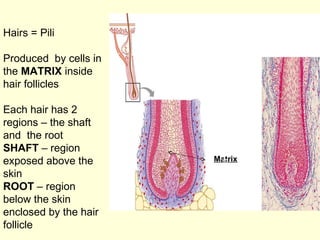
The integumentary system has two main divisions - the skin and accessory structures. The skin is the largest organ and has two layers, the epidermis and dermis. Accessory structures include sweat and sebaceous glands, hair follicles, and nails, which are derived from the epidermis.
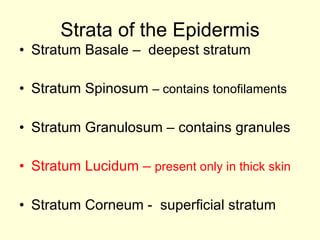
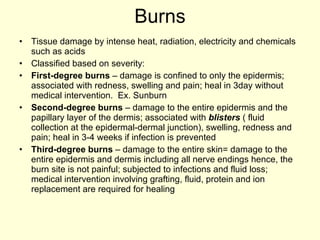
The epidermis has several strata with different cell types and densities. The dermis lies below with two layers - a papillary layer interdigitated with the epidermis and a deeper reticular layer. Various sensory receptors are located within the skin layers.
The skin has