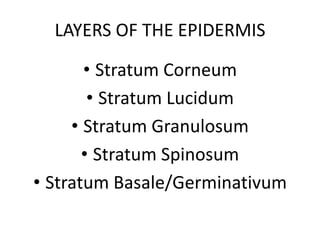
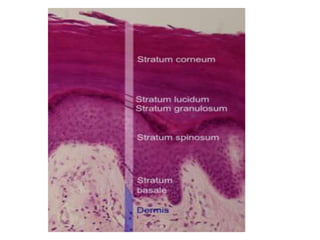
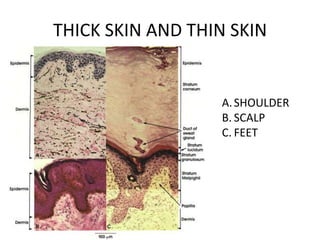
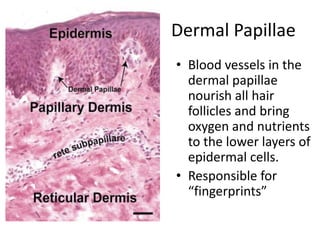
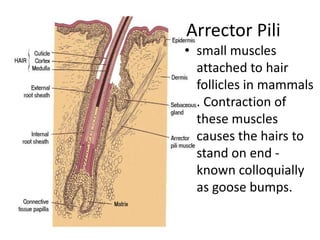
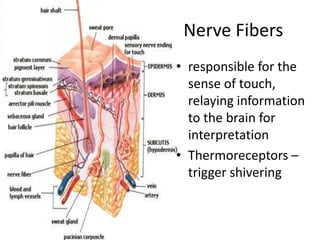
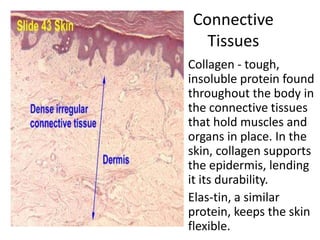
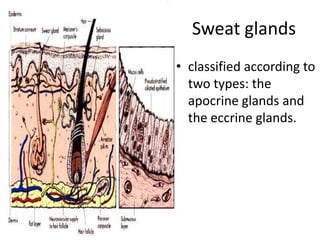
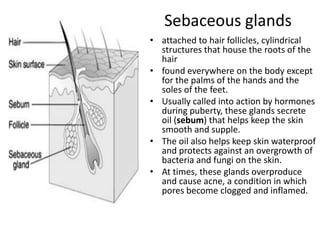
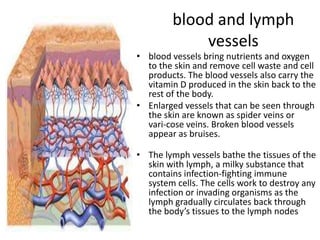
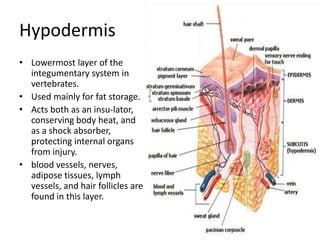
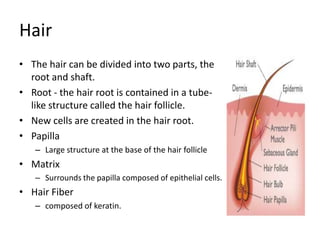
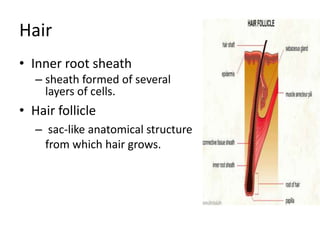
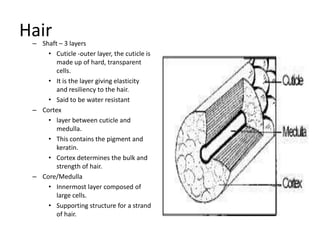
The epidermis is the outermost layer of skin composed of keratinocytes and other cell types. It forms a protective barrier against pathogens and regulates water loss. The epidermis consists of several layers - the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. The dermis lies beneath the epidermis and contains structures like hair follicles, sweat and oil glands, blood vessels, nerves. The hypodermis is the lowest layer and stores fat. Together these layers comprise the integumentary system which acts as a protective barrier for the body.